Abstract
CONTEXT: The impact of national efforts to limit antibiotic prescribing has not been fully evaluated.
OBJECTIVES: To analyze trends in outpatient visits associated with antibiotic prescription for U.S. adults.
DESIGN: Cross-sectional study of data (1995 to 2002) from the National Ambulatory Medical Care Survey and the National Hospital Ambulatory Medical Care Survey.
PARTICIPANTS: Adults ≥18 years with an outpatient visit to an office-or hospital-based medical practice or to an emergency department. All visits were classified into 1 of 4 diagnostic categories: (1) acute respiratory infection (ARI)—antibiotics rarely indicated, (2) ARI—antibiotics often indicated, (3) nonrespiratory infection—antibiotics often indicated, and (4) all others.
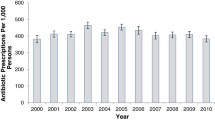
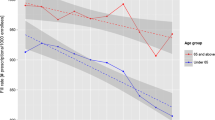
MEASUREMENTS: Trends in: (1) Proportion of outpatient visits associated with an antibiotic prescription; (2) proportion of antibiotic prescriptions that were broad spectrum; and (3) number of visits and antibiotic prescriptions per 1,000 U.S. adults ≥18 years of age.
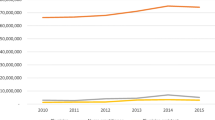
RESULTS: From 1995–1996 to 2001–2002, the proportion of all outpatient visits that generated an antibiotic prescription decreased from 17.9% to 15.3% (adjusted odds ratio [OR] 0.84, 95% confidence interval [CI] 0.76 to 0.92). The entire reduction was because of a decrease in antibiotic prescriptions associated with visits for ARIs where antibiotics are rarely indicated from 59.9% to 49.1% (adjusted OR 0.64 95% CI 0.51 to 0.80). However, the proportion of prescribed antibiotics for these visits that were classified as broad-spectrum antibiotic prescription increased from 41.0% to 76.8%. Overall outpatient visits increased from 1693 to 1986 per 1,000 adults over the 8 years studied, but associated antibiotic prescriptions changed little, from 302 to 304 per 1,000 adults.
CONCLUSION: During the study period, outpatient antibiotic prescribing for respiratory infections where antibiotics are rarely indicated has declined, while the proportion of broad-spectrum antibiotics prescribed for these diagnoses has increased significantly. This trend resulted in a 15% decline in the total proportion of outpatient visits in which antibiotics were prescribed. However, because outpatient visits increased 17% over this time period, the population burden of outpatient antibiotic prescriptions changed little.
Similar content being viewed by others
References
Arroll B, Kenealy T. Antibiotics for the common cold. Cochrane Database Syst Rev. 2002;CD000247.
Thomas MG, Arroll B. “Just say no”—reducing the use of antibiotics for colds, bronchitis and sinusitis. N Z Med J. 2000;113:287–9.
McGowan JE Jr. Economic impact of antimicrobial resistance. Emer Infect Dis. 2001;7:286–92.
Bertino JS. Cost burden of viral respiratory infections: issues for formulary decision makers. Am J Med. 2002;112(suppl 6A):42S-9S.
McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA. 1995;273:214–9.
Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278:901–4.
Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. JAMA. 2003;289:719–25.
Steinman MA, Gonzales R, Linder JA, Landefeld CS. Changing use of antibiotics in community-based outpatient practice, 1991–1999. Ann Intern Med. 2003;138:525–33.
Mainous AG III, Hueston WJ, Davis MP, Pearson WS. Trends in antimicrobial prescribing for bronchitis and upper respiratory infections among adults and children. Am J Public Health. 2003;93:1910–4.
Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics. 2001;108:1–7.
Gonzales R, Steiner JF, Lum A, Barrett PH Jr. Decreasing antibiotic use in ambulatory practice: impact of a multidimensional intervention on the treatment of uncomplicated acute bronchitis in adults. JAMA. 1999;281:1512–9.
Perz JF, Craig AS, Coffey CS, et al. Changes in antibiotic prescribing for children after a community-wide campaign. JAMA. 2002;287:3103–9.
Get smart know when antibiotics work. Centers for Disease Control and Prevention; Available at: http://www.cdc.gov/drugresistance/community/Accessed February 15, 2005.
Snow V, Mottur-Pilson C, Gonzales R. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults. Ann Intern Med. 2001;134:487–9.
Snow V, Mottur-Pilson C, Gonzales R. Principles of appropriate antibiotic use for treatment of acute bronchitis in adults. Ann Intern Med. 2001;134:518–20.
Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: background. Ann Intern Med. 2001;134:521–9.
Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of acute respiratory tract infections in adults: background, specific aims, and methods. Ann Intern Med. 2001;134:479–86.
Gonzales R, Bartlett JG, Besser RE, Hickner JM, Hoffman JR, Sande MA. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults: background. Ann Intern Med. 2001;134:490–4.
NAMCS. Available at: http://www.cdc.gov/nchs/about/major/ahcd/namcsds.htm. Accessed February 15, 2005.
NHAMCS. Available at: http://www.cdc.gov/nchs/about/major/ahcd/nhamcsds.htm. Accessed February 15, 2005.
US Population Estimates. Available at: http://www.census.gov/population/www/estimates/uspop.html. Accessed February 15, 2005.
International Classification of Diseases, Ninth Revision, Clinical Modification. Washington, DC: Public Health Service, US Department of Health and Human Services; 1988.
Snow V, Lascher S, Mottur-Pilson C. The evidence base for management of acute exacerbations of COPD: clinical practice guideline, part 1. Chest. 2001;119:1185–9.
Peng CC, Aspinall SL, Good CB, Atwood CW Jr., Chang CC. Equal effectiveness of older traditional antibiotics and newer broad-spectrum antibiotics in treating patients with acute exacerbations of chronic bronchitis. South Med J. 2003;96:986–91.
Adams SG, Melo J, Luther M, Anzueto A. Antibiotics are associated with lower relapse rates in outpatients with acute exacerbations of COPD. Chest. 2000;117:1345–52.
Eltinge JL, Sribney WM. Estimates of linear combinations and hypothesis tests for survey data. Stata Tech Bull. 1996;31:31–42, 246–59.
Reed SD, Laxminarayan R, Black DJ, Sullivan SD. Economic issues and antibiotic resistance in the community. Ann Pharmacother. 2002;36:148–54.
Vogel RJ, Ramachandran S, Zachry WM. A 3-stage model for assessing the probable economic effects of direct-to-consumer advertising of pharmaceuticals. Clin Ther. 2003;25:309–29.
McCaig LF, Besser RE, Hughes JM. Antimicrobial drug prescription in ambulatory care settings, United States, 1992–2000. Emerg Infect Dis. 2003;9:432–7.
Halasa NB, Griffin MR, Zhu Y, Edwards KM. Decreased number of antibiotic prescriptions in office-based settings from 1993 to 1999 in children less than five years of age. Pediatr Infect Dis J. 2002;21:1023–8.
Finkelstein JA, Stille C, Nordin J, et al. Reduction in antibiotic use among US children, 1996–2000. Pediatrics. 2003;112(3 Part 1):620–7.
Molstad S, Cars O. Major change in the use of antibiotics following a national programme: Swedish Strategic Programme for the Rational Use of Antimicrobial Agents and Surveillance of Resistance (STRAMA). Scand J Infect Dis. 1999;31:191–5.
O’Brien KL, Santosham M. Potential impact of conjugate pneumococcal vaccines on pediatric pneumococcal diseases. Am J Epidemiol. 2004;159:634–44.
Amsden GW. Pneumococcal resistance in perspective: how well are we combating it? Pediatr Infect Dis J. 2004;23(2 Suppl):S125–8.
Jenson HB, Baltimore RS. Impact of pneumococcal and influenza vaccines on otitis media. Curr Opin Pediatr. 2004;16:58–60.
Talbot TR, Poehling KA, Hartert TV, et al. Reduction in high rates of antibiotic-nonsusceptible invasive pneumococcal disease in tennessee after introduction of the pneumococcal conjugate vaccine. Clin Infect Dis. 2004;39:641–8.
Talbot TR, Poehling KA, Hartert TV, et al. Elimination of racial differences in invasive pneumococcal disease in young children after introduction of the conjugate pneumococcal vaccine. Pediatr Infect Dis J. 2004;23:726–31.
Subcommittee on Otitis Media with Effusion. Clinical practice guideline from American Academy of Otolaryngology—Head and Neck Surgery and American Academy of Pediatics Subcommittee on Otitis Media with Effusion. Pediatrics. 2004;113:1412–29.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. Edwards has received grants from Aventis, VaxGen, and GlaxoSmithKline. Dr. Griffin has consulted for Merck and received a grant from Pfizer.
This material is based upon work supported by the Veterans Affairs Clinical Research Center of Excellence (CRCoE)(C. L. R., M. R. G.).
Public Health Service award K12 RR017697 for the Vanderbilt Mentored Clinical Research Scholar Program (N. B. H.).
Vanderbilt Center for Education and Research Vanderbilt Center for Education and Research on Therapeutics, Vanderbilt University School of Medicine (M. R. G.).
Geriatric Research Education and Clinical Center, Veterans Affairs, Tennessee Valley Healthcare System, Nashville, Tenn (C. L. R., M. R. G., R. S. D.)
General Clinical Research Center, Vanderbilt University School of Medicine, Nashville, Tenn (K. M. E.).
Rights and permissions
About this article
Cite this article
Roumie, C.L., Halasa, N.B., Grijalva, C.G. et al. Trends in antibiotic prescribing for adults in the United States—1995 to 2002. J Gen Intern Med 20, 697–702 (2005). https://doi.org/10.1111/j.1525-1497.2005.0148.x
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1111/j.1525-1497.2005.0148.x