Abstract
Objective: To search for major gaps in medication-taking behavior predisposing patients to cardiovascular morbidity and mortality.
Design: Convenience sample; cohort prospectively followed for ≤5 months.
Setting: General internal medicine and cardiology clinics in a university medical center.
Patients: From among 893 patients, the authors identified 132 eligible individuals and entered 33 subjects (25%) with chronic cardiovascular conditions, 1–3 chronic oral medications for these conditions, overall regimen of ≤6 drugs, regular visits at 1–3-month intervals, literacy in English, willingness to use electronic monitors, and physician permission to participate.
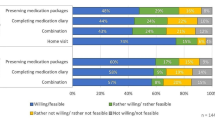
Outcome measures: Medication compliance rates and patterns by patient self-report, physician estimates, pill count, and electronic monitoring of pill vial opening.
Results: Despite moderately complex regimens (5.4±0.5 pills daily; range 1–11), most subjects took most medications according to the prescription: median intervals between pill vial openings were 1.00, 0.50, and 0.43 days for once, twice, and three times daily dosing, respectively. Medication-taking gaps of ≥2 times the prescribed interdosing interval occurred for 48% of the patients. Patients’ dosing patterns often produced “uncovered” intervals (mean duration 3.7 days, range 0–25) with doubtful pharmacologic effectiveness. These lapses were underestimated by patients and poorly perceived by their treating physicians, despite familiarity with their care. Baseline sociodemographic, psychosocial, medical system, or clinical characteristics did not predict the patterns or degrees of medication noncompliance.
Conclusions: Major treatment gaps occur frequently, even in carefully selected ambulatory populations, and generally escape detection. The compliance patterns and gaps may contribute to reported excesses of cardiovascular morbidity and mortality.
Similar content being viewed by others
References
Mushlin AI, Appel FA. Diagnosing patient noncompliance. Arch Intern Med. 1977;137:318–21.
Gilbert JR, Evans CE, Haynes RB, Tugwell P. Predicting compliance with a regimen of digoxin therapy in family practice. Can Med Assoc J. 1980;123:119–22.
Caron HS. Compliance: the case for objective measurement. J Hypertens. 1985;3(suppl 1):11–7.
Kass MA, Gordon M, Meltzer DW. Can ophthalmologists correctly identify patients defaulting from pilocarpine therapy? Am J Ophthalmol. 1986;101:524–30.
Eisen SA, Woodward RS, Miller D, Spitznagel E, Windham CA. The effect of medication compliance on the control of hypertension. J Gen Intern Med. 1987;2:298–305.
Cramer JA, Mattson RH, Prevey ML, Scheyer RD, Ouellette VL. How often is medication taken as prescribed? A novel assessment technique. JAMA. 1989;261:3273–7.
Rudd P, Byyny RL, Zachary V, et al. The natural history of medication compliance in a drug trial: limitations of pill counts. Clin Pharmacol Ther. 1989;46:169–76.
Cramer JA, Scheyer RD, Mattson RH. Compliance declines between clinic visits. Arch Intern Med. 1990;150:1509–10.
Eisen SA, Miller DK, Woodward RS, Spitznagel E, Przybeck TR. The effect of prescribed daily dose frequency on patient medication compliance. Arch Intern Med. 1990;150:1881–4.
Kruse W, Weber E. Dynamics of drug regimen compliance—its assessment by microprocessor-based monitoring. Eur J Clin Pharmacol. 1990;38:561–5.
Rudd P, Ahmed S, Zachary V, Barton C, Bonduelle D. Improved compliance measures: applications in an ambulatory hypertensive drug trial. Clin Pharmacol Ther. 1990;48:676–85.
Rudd P, Marshall G. Resolving problems of measuring compliance with medication monitors. J Compliance Health Care. 1987;2:23–35.
Maronde RF, Chan LS, Larsen FJ, Strandberg LR, Laventurier MF, Sullivan SR. Underutilization of antihypertensive drugs and associated hospitalization. Med Care. 1989;27:1159–66.
Psaty BM, Koepsell TD, Wagner ED, LoGerfo JP, Inui TS. The relative risk of incident coronary heart disease associated with recently stopping the use of beta-blockers. JAMA. 1990;263:1653–7.
Shope JT. Compliance in children and adults: review of studies. Epilepsy Res. 1988;1(suppl 23):23–47.
Knight RA, Hay DA. The relevance of the health belief model to Australian smokers. Soc Sci Med. 1989;28:13H-4.
Rangno RE, Langlois S. Comparison of withdrawal phenomena after propranolol, metoprolol and pindolol. Br J Clin Pharmacol. 1982;13(suppl 2):345S-351S.
Houston MC, Hodge R. Beta-adrenergic blocker withdrawal syndromes in hypertension and other cardiovascular diseases. Am Heart J. 1988;116:515–23.
Gilligan DM, Chan WL, Stewart R, Oakley CM, Krikler S, Joshi J. Adrenergic hypersensitivity after beta-blocker withdrawal in hypertrophic cardiomyopathy. Am J Cardiol. 1991;68:766–72.
Rudd P. Blood pressure reduction and the risk of myocardial infarction. JAMA. 1990;263:660.
Cruickshank JM. Coronary flow reserve and the J curve relation between diastolic blood pressure and myocardial infarction. BMJ. 1988;297:1227–30.
Alderman MH, Ooi WL, Madhavan S, Cohen H. Treatment-induced blood pressure reduction and the risk of myocardial infarction. JAMA. 1989;262:920–4.
Berglund G. Goals of antihypertensive therapy: is there a point beyond which pressure reduction is dangerous? Am J Hypertens. 1989;2:586–98.
Kass MA, Meltzer DW, Gordon M, Cooper D, Goldberg J. Compliance with topical pilocarpine treatment. Am J Ophthalmol. 1986;101:515–23.
Gordon ME, Kass MA. Validity of standard compliance measures in glaucoma compared with an electronic eyedrop monitor. In: Cramer JA, Spilker B (eds). Patient Compliance in Medical Practice and Clinical Trials. New York: Raven Press, 1991;163–73.
Cramer JA, Mattson RH. Monitoring compliance with antiepileptic drug therapy. In: Cramer JA, Spilker B (eds). Patient Compliance in Medical Practice and Clinical Trials. New York: Raven Press, 1991; 123–37.
Johnston GD, Kelly JG, McDevitt DG. Do patients take digoxin? Br Heart J. 1978;40:1–7.
Squire A, Goldman ME, Kupersmith J, Stern EH, Fuster V, Schweitzer P. Long-term antiarrhythmic therapy. Problem of low drug levels and patient noncompliance. Am J Med. 1984;77:1035–8.
Col N, Fanale JE, Kronholm P. The role of medication noncompliance and adverse drug reactions in hospitalizations of the elderly. Arch Intern Med. 1990;150:841–5.
Sampson JJ, Arbona CL. Causes and effects of noncompliance in cardiac patients. Clin Cardiol. 1980;3:207–10.
Levine AM, Richardson JL, Marks G, et al. Compliance with oral drug therapy in patients with hematologic malignancy. J Clin Oncol. 1987;5:1469–76.
Richardson JL, Shelton DR, Krailo M, Levine AM. The effect of compliance with treatment on survival among patients with hematologic malignancies. J Clin Oncol. 1990;8:356–64.
Didlake RH, Dreyfus K, Kerman RH, Van Buren CT, Kahan BD. Patient noncompliance: a major cause of late graft failure in cyclosporine-treated renal transplants. Transplant Proc. 1988;20(suppl 3):63–9.
Rovelli M, Palmeri D, Vossler E, Bartus S, Hull D, Schweizer R. Noncompliance in organ transplant recipients. Transplant Proc. 1989;21(1):833–4.
Schweizer RT, Rovelli M, Palmeri D, Vossler E, Hull D, Bartus S. Noncompliance in organ transplant recipients. Transplantation. 1990;49(2):374–7.
Muller JE, Tofler GH, Willich SN, Stone PH. Circadian variation of cardiovascular disease and sympathetic activity. J Cardiovasc Pharmacol. 1987;10(suppl 2):S104-S109.
Muller JE, Tofler GH, Stone PH. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation. 1989;79:733–43.
Tofler GH, Stone PH, Maclure M, et al. Analysis of possible triggers of acute myocardial infarction (the MILIS study). Am J Cardiol. 1990;66:22–7.
Rudd P, Ahmed S, Zachary V, Barton C, Bonduelle D. Compliance with medication-timing: implications from a medication trial for drug development and clinical practice. J Clin Res Pharmacoepidemiol. 1992;6(3):15–27.
Rudd P, Ahmed, S, Zachary V, Barton C, Bonduelle D. Issues in patient compliance: the search for therapeutic sufficiency. Cardiology. 1992;80(suppl 1):2–10.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Rudd, P., Ramesh, J., Bryant-Koslinc, C. et al. Gaps in cardiovascular medication taking. J Gen Intern Med 8, 659–666 (1993). https://doi.org/10.1007/BF02598282
Issue Date:
DOI: https://doi.org/10.1007/BF02598282