Abstract
Purpose
To examine the natural course and outcome of major depressive disorder (MDD) in primary care over 39 months.
Methods
Prospective cohort study of 1,338 consecutive attendees with follow-up after 6, 12, and 39 months with DSM-IV MDD using the Composite International Diagnostic Interview (CIDI). We measured severity of depressive symptoms (Patient Health Questionnaire 9), somatic symptoms (Patient Health Questionnaire 15), and mental and physical function (Short Form 12, mental and physical component summary). Analysis of variance and random coefficient models were performed.
Results
At baseline, 174 people (13%) had MDD of which 17% had a chronic and 40% had a fluctuating course, while 43% remitted. Patients with chronic courses had more severe depressive symptoms (mean difference 6.54; 95% CI 4.38–8.70), somatic symptoms (mean difference 3.31; 95% CI 1.61–5.02), and greater mental dysfunction (mean difference −10.49; 95% CI −14.42 to −6.57) at baseline than those who remitted from baseline, independent of age, sex, level of education, presence of a chronic disease, and a lifetime history of depression.
Conclusions
Although 43% of patients with MDD attending primary care recover, this leaves a majority of patients (57%) who have a chronic or intermittent course. Chronic courses are associated with higher levels of depressive symptoms and somatic symptoms and greater mental dysfunction at baseline.
Similar content being viewed by others
Introduction
Major depressive disorder (MDD) is a serious health problem and will be the second leading cause of burden of disease worldwide by 2030 [1]. In any given 12-month period, 10–20% of adults will visit their general practitioner (GP) for mental complaints, of which the majority are related to depression [2]. The prevalence of MDD in primary care is estimated to be between 4 and 18% [3]. People presenting with depressive symptoms are mainly seen in primary care; however, treatment guidelines are mainly based upon data from hospital settings or the general population [4]. Few studies have examined the course and outcome of MDD in primary care over a greater period of time. In one study, 32% of the primary care patients who were depressed at baseline were not depressed after 12 months and 47% were not depressed after 3.5 years [5]. A recent study showed that of the 79 primary care patients diagnosed with MDD at baseline, 25% persisted and 49% suffered from residual symptoms or recurrences after 18 months [6]. These data suggest that the majority of adult patients with depression in primary care do not recover in the medium-term, but also that some patients do recover.
Most of the observational cohort studies of depression in primary care included small sample sizes and had a short duration of follow-up [4, 7]. The nature of depression can be complex: symptoms can improve and deteriorate over time and patients can switch between depression categories [4]. However, this fluctuating course of depression can be missed in studies with a short duration of follow-up or few assessments [8]. A recent review showed that between 1985 and 2006 only two observational studies in primary care were performed with a follow-up longer than one year [4]. These studies included three assessments of depression at most.
The objective of this study was to examine the natural course of MDD in primary care attendees over a period of 39 months. We investigated the course of major depression and its relationship to the severity of depressive and somatic symptoms, and mental and physical function in a cohort of primary care attendees aged 18 years or older who were diagnosed with MDD at baseline.
Methods
Study setting and design
PredictD is a multicenter prospective cohort study from which a multifactor algorithm was developed to predict risk of onset of MDD in primary care patients in six European countries and Chile [3, 9–11]. In brief, in 2003, consecutive adult primary care patients were asked to participate, irrespective of their reasons for consulting their general practitioners. Patients were followed-up after 6 and 12 months. The current study used data from PREDICT-NL, the Dutch part of PredictD, in which an additional follow-up after 39 months was conducted. The study was approved by the medical ethics committee of the University Medical Center Utrecht and was conducted in seven large general practice centres near Utrecht.
Study participants
Consecutive attendees aged 18 years or older were recruited and interviewed between April 2003 and September 2004. Patients willing to participate were asked to fill in risk factor questionnaires and sign informed consent within 2 weeks. After the risk factor questionnaires were returned, an appointment was made by the researchers to conduct a diagnostic depression interview at the general practice. If patients did not respond after 2 weeks, a first reminder was sent and, if necessary, a second reminder after 4 weeks. Participants who did not respond to the second reminder were considered to be non-responders. All participants gave written informed consent.
Diagnosis of major depressive disorder
The diagnosis of MDD was assessed in all patients according to DSM-IV criteria using the depression section of the Composite International Diagnostic Interview (CIDI) [12, 13]. The researchers contacted the participant by telephone and asked the two core questions of the depression section of the CIDI interview (depressed mood or a loss of interest). MDD was defined as absent if the participant responded negatively to both questions [12]. If the participant responded positively to either question, an appointment was made in the general practice to conduct the entire depression section of the CIDI interview. The interviewers were blinded to the answers on the risk factor questionnaires. At baseline, the 6- and 12-month follow-up, diagnosis of MDD was assessed covering the preceding 6 months. At the 39-month follow-up, diagnosis of MDD was assessed covering the period between the 12- and 39-month follow-up. If the participant was unable to schedule the interview at the general practice, the interview was done through telephone (23% of interviews at baseline, 17% at the 6-month follow-up, and 19% at the 12-month follow-up). At the 39-month follow-up, all interviews were through telephone. Several studies have shown that both methods are comparable with respect to validity and reliability [14].
Outcome measures
Severity of depressive symptoms
The self-report Patient Health Questionnaire 9 (PHQ-9) was included with the risk factor questionnaires [15]. It assesses the presence in the past 2 weeks of the nine DSM-IV criteria for MDD on a 4-point rating scale, ranging from 0 (“not at all”) to 3 (“nearly every day”). The scores on this questionnaire range from 0 to 27.
Severity of somatic symptoms
Severity of somatic symptoms was assessed by the PHQ-15, which inquires about 15 somatic symptoms in the preceding 4 weeks: (1) stomach pain, (2) back pain, (3) pain in your arms, legs, or joints, (4) menstrual cramps or other problems with your periods (women only), (5) headaches, (6) chest pain, (7) dizziness, (8) fainting spells, (9) feeling your heart pound or race, (10) shortness of breath, (11) pain or problems during sexual intercourse, (12) constipation, loose bowels, or diarrhoea, (13) nausea, gas, or indigestion, (14) feeling tired or having low energy, and (15) trouble sleeping [16]. It uses a 3-point rating scale, ranging from 0 (“not bothered at all”) to 2 (“bothered a lot”). The scores on this questionnaire range from 0 to 30.
Mental and physical functions
Mental and physical functions were assessed by the Short Form 12 (SF-12 MCS and PCS) [17]. The SF-12 is derived from the SF-36, both of which have been widely used in primary care settings. The SF-12 yields a scale from 0 to 100, in which lower scores indicate greater dysfunction.
Other variables
Patient characteristics were obtained at baseline using self-report questionnaires and included age, sex, employment status (employed or unemployed), marital status (living with or without a partner), educational level (11-point ordinal scale ranging from ‘no education’ to ‘PhD-level’, categorized into lower, middle, and higher level of education), number of life events (no, one, or two or more events), and presence of one or more chronic diseases diagnosed by a physician [18]. Lifetime depression was based on affirmative answers to both of the first two questions of the CIDI depression section [19].
Data analysis
Missing data rarely occurs completely at random and a complete case analysis may lead to loss of statistical power and to biased results [20]. We, therefore, used multiple imputations to address missing data which were imputed at baseline, at the 6-, 12-, and 39-month follow-up separately [21]. At each time-point 10 datasets were generated and all variables mentioned above were used as predictors. We compared results obtained by analysing with and without imputation to observe the extent of imputation used.
First, baseline characteristics before imputation for participants with and without MDD were presented as means with standard deviations (SD) for continuous variables and numbers with percentages for categorical variables, and tested with F-tests (ANOVA) and the Chi-squared tests, respectively. Missing data for each covariate at baseline are presented.
Second, a flowchart was created to describe the course of participants with MDD at baseline. At each assessment, we calculated the number of lost to follow-up. The flowcharts categorized participants into different courses. We defined the following three courses: (1) patients who were in remission from baseline (remitted); (2) patients who had a fluctuating MDD course (intermittent); and (3) patients who had MDD at all four assessments (chronic).
Third, for each outcome variable (PHQ-9, PHQ-15, SF-12 MCS, and PCS) separate analysis of variance (ANOVA) was performed with the scores at each assessment as dependent and the course groups as independent variable. We used ANOVA analyses to test for differences in mean symptom or function score among each course group.
Fourth, SAS PROC MIXED was used in random coefficient analyses (RCA) with robust standard errors, to estimate the change in depressive symptoms, somatic symptoms, mental function, and physical function over time for each course group. We used random intercept and slope for best model fit. The courses and time, and the interaction between course group and time were entered as independent variables and the outcome measure was entered as the dependent variable. The coefficients of interaction between the course groups and time represent the change of symptom or function over time as a function of the course group. The time between the follow-up assessments was computed for each person individually. Age, sex, education level, presence of a chronic disease, and lifetime depression were added to the models to control for potential confounding. Analyses were performed using PASW version 17 (IBM SPSS Statistics) and SAS version 9.1 (SAS institute).
Results
In total, 3,089 patients were asked to take part in the study, of which 83 did not meet inclusion criteria. Seventy-five were not fluent in Dutch, five had dementia, two had psychosis, and one had severe learning disabilities. Of the remaining 3,006 patients, 1,338 (44.5%) consented and took part in the study, while 915 (30%) actively refused. Reasons for not participating were mostly lack of time (21%, N = 192) and no interest (24%, N = 224). Refusal without reason was present in 249 (8%) with and 504 (16%) without demographic information. Of the 1,164 refusals on whom we had demographic information, we found no difference in the age (mean 51 years, SD 19) and sex (62% female) distribution when compared to our participants. The numbers lost to follow-up throughout the study period were similar amongst participants who were depressed at baseline (74/174, 43%) and those who were not depressed (504/1,164, 43%). Participants who were lost to follow-up were similar in age and sex distribution, baseline PHQ-9, PHQ-15, SF-12 MCS, and PCS scores to those who were retained in the study.
Of the 1,338 participants, 1,266 (95%) participated at the 6-month follow-up, and 1,206 (95% of 1,266) at 12 months. At 39 months, 1,133 participants were invited to take part, because 72 participants withdrew from the study and one participant died. Of the 1,133 invited participants, 759 participants consented to take part (67%). The mean durations of follow-up in months were 5.7 (SD 0.6) at the 6-month follow-up, 12.0 (SD 0.6) at 12 months and 39.2 (SD 2.3) at 39 months. The cohort was mainly female (63%) and middle-aged (mean 51 years, SD 17), and most of them were living with a partner (75%) (Table 1).
After imputation of missing values, at baseline the prevalence of MDD over the previous 6 months was 13.0% (N = 174), 9.0% (N = 115) at 6 months, and 5.5% (N = 67) at 12 months. At 39 months, 11.8% (N = 90) had MDD in the period between 12- and 39-months assessment. Of the 174 participants who were depressed at baseline, 100 were followed up at all three time points (Fig. 1). As much as 43% of the participants with MDD at baseline were in remission from baseline, 40% had a fluctuating course of depression, while 17% were chronically depressed over the 39 months of the study (Table 2).
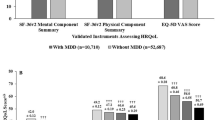
We present unadjusted mean depressive and somatic symptom levels at each assessment for the three course groups in Figs. 2 and 3, and mean mental and physical function scores in Figs. 4 and 5. Participants with a chronic course of disease had a higher level of depressive and somatic symptoms and greater mental and physical dysfunction over time compared to the other courses. However, the difference of physical function among all courses over time was little. Participants who remitted from baseline had a lower level of depressive and somatic symptoms and less mental dysfunction over time when compared to the other course groups. Complete case analysis before imputation for PHQ-9 (N = 75), PHQ-15 (N = 79), SF-12 MCS, and PCS (both N = 64) revealed similar results.
Severity of depressive and somatic symptoms decreased and mental function increased over time in participants with MDD at baseline (Table 3). When compared to participants who remitted from baseline, people with a chronic course had significantly higher levels of depressive and somatic symptoms and greater mental dysfunction at baseline, after adjustment for age, sex, education, presence of a chronic disease, and lifetime depression. The severity of symptoms and function for those with a chronic course did not significantly change over time compared to those who were in remission from baseline. Physical function was similar in all course groups. Analysis before imputation (N = 85) for PHQ-9, PHQ-15, SF-12 MCS, and PCS did affect the estimates, but did not lead to other conclusions.
Discussion
Our study examined the natural course and outcome of MDD in adult primary care attendees. We observed that 17% of participants with MDD at baseline continued to be depressed after 39 months, and another 40% had a fluctuating course of depression, while 43% were in remission from baseline. Participants with a chronic course of MDD had more depressive and somatic symptoms and greater mental dysfunction at baseline, independent of age, sex, level of education, presence of a chronic disease, and lifetime depression compared to those who remitted from baseline.
To our knowledge, this is one of the few observational studies on the natural course of MDD in primary care attendees with a medium-term follow-up and more than two assessments. Previous work is mainly restricted to specialty mental health care clinics or general population samples despite the fact that most people with depression and anxiety are managed in primary care [22]. Unlike previous research, our study had a relatively long follow-up period during which we conducted several assessments. Furthermore, we had a medium-sized sample of 174 persons with MDD at baseline which we diagnosed using DSM-IV criteria rather than relying on cross-sectional questionnaires.
However, our study was limited by low response rates at baseline, although similar participation rates have been found in other observational studies in primary care [10, 23]. This could be partly explained by the fact that people were recruited to the study by researchers in the waiting room rather than by the consulting physicians. Given the relatively high prevalence of MDD at baseline, it is possible that persons with MDD were more willing to participate. Nevertheless, loss to follow-up was extremely low during the first 12 months, and during the entire follow-up period loss to follow-up in those depressed or not depressed at baseline was similar. Second, the time between 12 and 39 months was longer than in between the other assessments. Consequently, participants were asked about their symptoms retrospectively in the preceding 2 years and 3 months during the final follow-up, which might have been less reliable than for the other follow-up assessments. Third, since we did not have data on treatments received for depression we could not analyse the influences of these on the course of the illness. Nevertheless, these results still reflect the longitudinal history of MDD in people seen in general practice over time. Fourth, primary care is not uniformly organized in all countries, so these findings might not be generalizable to all countries.
The majority of participants who were diagnosed with MDD at baseline had an intermittent or chronic course of disease. Our findings are concordant with several community-based studies with follow-up durations ranging from 2 to 49 years in adults diagnosed with MDD showing that about 20% developed a chronic course and about 30–50% had a recurrent course [24–29]. Our findings suggest that the natural history of depression in primary care resembles that of depression in the general adult population.
As much as 57% of patients diagnosed with MDD at baseline had not recovered after 39 months, which is consistent with findings from a study in primary care with three assessments, where 53% of the adult population diagnosed with MDD at baseline had not recovered after 3.5 years, in which partial remission rather than full recovery was the rule [5, 30]. Two methodological differences between their study and the present study are noteworthy. First, the latter study used a two-stage design in which consecutive primary care attendees were screened on psychiatric illness by their consulting physicians and by the researchers using the General Health Questionnaire (GHQ). Subsequently, a stratified random sample was selected for the baseline examination on the basis of the outcome of this GP and GHQ screening. In our study, consecutive primary care attendees were included irrespective of their reasons for consulting the GP. Second, those who were included in the study by Ormel et al. were diagnosed using the Present State Examination (PSE), while we diagnosed MDD using the CIDI. Disability was measured by the Groningen Social Disability Schedule (SDS) in their study compared to the SF-12 used in our study. We have built on their study by including a larger sample of primary care attendees, who were included irrespective of their reason for consultation. Although the methods employed in our study were somewhat different, the results were generally comparable and support the finding that the majority of those diagnosed with MDD have a poor course. As much as 17% in our study had MDD at all assessments, which is lower than results from a primary care study of 160 patients diagnosed with MDD at baseline, of which 32% had not recovered at 3 years [31]. However, the latter study was performed in a sample of older people making direct comparisons difficult. Recent primary care-based studies revealed that about 50% of depressed adolescents failed to recover after 6 months, while 74% of depressed adults had not recovered after 18 months [6, 32]. In addition, the recurrence rate of primary care depression may be up to 64% over a period of 23 years [33].
Participants with a chronic course had more depressive and somatic symptoms and greater mental dysfunction at baseline than those remitted from baseline. Baseline severity of depression is a risk factor for persistence in the short-term, as shown by other studies, but our findings suggest that it is also a risk factor for persistence in the medium-term, even independent of a depression history [34, 35]. The latter has also recently been shown by a primary care study which followed recurrent depressive patients for 3 years, and our results underline these findings [36]. The study by Ormel et al. [5] reported that patients with depression who had higher levels of disability improved considerably over time, although residual disability was present in some cases. A relationship between somatic symptoms and depression, and between mental dysfunction and depression severity has been found in cross-sectional studies in primary care, but our results add to the current knowledge that high levels of somatic symptoms and greater mental dysfunction at baseline are possible risk factors for persistence of depression over 39 months [37, 38]. Within the chronic group, the level of depressive and somatic symptoms and mental functioning did not change over time compared to those who remitted from baseline, suggesting that those who are depressed and have higher symptom levels or lower levels of function at baseline are likely to persist in higher levels of symptoms and lower levels of function over the course of 39 months.
Findings from the current study suggest that for those attending primary care, a higher severity of depressive or somatic symptoms, or lower levels of mental function may be an indication of a poor course of MDD. The pattern of depressive and somatic symptoms over time for the course groups was similar to the pattern of mental function over time, which may suggest that depressive symptoms, somatic symptoms, and mental function are related. Since we did not have premorbid functioning data available, we were unable to determine whether trait or scar effects were present [39]. Although we cannot confirm the presence of a state effect within the course groups, as all participants improved significantly over time, synchrony of change between severity of depressive symptoms and severity of mental function may be present [39, 40]. Moreover, it is possible that synchrony of change between the severity of somatic symptoms and severity of mental function also exists. Therefore, depressive and somatic symptoms and mental function have to be monitored closely in primary care patients diagnosed with MDD as such surveillance could assist in the management and possible prevention of chronic depression.
The results of this study suggest that although 43% of patients with MDD attending primary care recover, this leaves a majority of patients (57%) who have a chronic or intermittent course. Persistence or chronicity of MDD is associated with the severity of depressive and somatic symptoms and mental dysfunction at baseline.
References
Mathers CD, Loncar D (2006) Projections of global mortality, burden of disease from 2002 to 2030. PLoS Med 3(11):e442
Kirmayer LJ, Robbins JM, Dworkind M et al (1993) Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry 150(5):734–741
King M, Nazareth I, Levy G et al (2008) Prevalence of common mental disorders in general practice attendees across Europe. Br J Psychiatry 192(5):362–367
Gilchrist G, Gunn J (2007) Observational studies of depression in primary care: what do we know? BMC Fam Pract 8:28
Ormel J, Oldehinkel T, Brilman E et al (1993) Outcome of depression and anxiety in primary care. A three-wave 3 1/2-year study of psychopathology and disability. Arch Gen Psychiatry 50(10):759–766
Vuorilehto MS, Melartin TK, Isometsa ET (2009) Course and outcome of depressive disorders in primary care: a prospective 18-month study. Psychol Med 2:1–11
Tiemens BG, Ormel J, Simon GE (1996) Occurrence, recognition, and outcome of psychological disorders in primary care. Am J Psychiatry 153(5):636–644
Licht-Strunk E, van der Windt DA, van Marwijk HW et al (2007) The prognosis of depression in older patients in general practice and the community. A systematic review. Fam Pract 24(2):168–180
King M, Weich S, Torres-Gonzalez F et al (2006) Prediction of depression in European general practice attendees: the PREDICT study. BMC Public Health 6(1):6
King M, Walker C, Levy G et al (2008) Development and validation of an international risk prediction algorithm for episodes of major depression in general practice attendees: the PredictD study. Arch Gen Psychiatry 65(12):1368–1376
Zuithoff NP, Vergouwe Y, King M et al (2009) A clinical prediction rule for detecting major depressive disorder in primary care: the PREDICT-NL study. Fam Pract 26(4):241–250
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders DSM-IV. American Psychiatric Publishing Inc.
World Health Organisation (1997) Composite International Diagnostic Interview (CIDI), version 2.1. WHO, Geneva
Rohde P, Lewinsohn PM, Seeley JR (1997) Comparability of telephone and face-to-face interviews in assessing axis I and II disorders. Am J Psychiatry 154(11):1593–1598
Spitzer RL, Kroenke K, Williams JB (1999) Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 282(18):1737–1744
Kroenke K, Spitzer RL, Williams JB (2002) The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med 64(2):258–266
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34(3):220–233
Brugha T, Bebbington P, Tennant C et al (1985) The list of threatening experiences: a subset of 12 life event categories with considerable long-term contextual threat. Psychol Med 15(1):189–194
Arroll B, Khin N, Kerse N (2003) Screening for depression in primary care with two verbally asked questions: cross sectional study. BMJ 327(7424):1144–1146
Donders AR, van der Heijden GJ, Stijnen T et al (2006) Review: a gentle introduction to imputation of missing values. J Clin Epidemiol 59(10):1087–1091
Engels JM, Diehr P (2003) Imputation of missing longitudinal data: a comparison of methods. J Clin Epidemiol 56(10):968–976
Culpepper L (2002) The active management of depression. J Fam Pract 51(9):769–776
Simon GE, Chisholm D, Treglia M et al (2002) Course of depression, health services costs, and work productivity in an international primary care study. Gen Hosp Psychiatry 24(5):328–335
Eaton WW, Shao H, Nestadt G et al (2008) Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry 65(5):513–520
Spijker J, de Graaf R, Bijl RV et al (2002) Duration of major depressive episodes in the general population: results from The Netherlands Mental Health Survey and Incidence Study (NEMESIS). Br J Psychiatry 181:208–213
van Weel-Baumgarten EM, Schers HJ, van den Bosch WJ et al (2000) Long-term follow-up of depression among patients in the community and in family practice settings. A systematic review. J Fam Pract 49(12):1113–1120
Rhebergen D, Beekman AT, de Graaf RD et al (2008) The three-year naturalistic course of major depressive disorder, dysthymic disorder and double depression. J Affect Disord 115(3):450–459
Mattisson C, Bogren M, Horstmann V et al (2007) The long-term course of depressive disorders in the Lundby Study. Psychol Med 37(6):883–891
Dowrick C, Shiels C, Page H et al (2009) Predicting long-term recovery from depression in community settings in Western Europe: evidence from ODIN. Soc Psychiatry Psychiatr Epidemiol [Epub ahead of print]
Brilman E, van den Brink W, Giel R et al (1992) Voorkomen en lange-termijnbeloop van psychische stoornissen in de huisartspraktijk. Tijdschrift voor Psychiatrie 34(6):385–399
Licht-Strunk E, van Marwijk HW, Hoekstra T et al (2009) Outcome of depression in later life in primary care: longitudinal cohort study with three years’ follow-up. BMJ 338:a3079
Gledhill J, Garralda ME. (2010) The short-term outcome of depressive disorder in adolescents attending primary care: a cohort study. Soc Psychiatry Psychiatr Epidemiol. [Epub ahead of print]
Yiend J, Paykel E, Merritt R et al (2009) Long term outcome of primary care depression. J Affect Disord 118(1–3):79–86
Barkow K, Maier W, Ustun TB et al (2003) Risk factors for depression at 12-month follow-up in adult primary health care patients with major depression: an international prospective study. J Affect Disord 76(1–3):157–169
Katon W, Lin E, Von Korff M et al (1994) The predictors of persistence of depression in primary care. J Affect Disord 31(2):81–90
Conradi HJ, de Jonge P, Ormel J (2007) Prediction of the three-year course of recurrent depression in primary care patients: different risk factors for different outcomes. J Affect Disord 105:267–271
Noel PH, Williams JW Jr, Unutzer J et al (2004) Depression and comorbid illness in elderly primary care patients: impact on multiple domains of health status and well-being. Ann Fam Med 2(6):555–562
Garcia-Campayo J, Ayuso-Mateos JL, Caballero L et al (2008) Relationship of somatic symptoms with depression severity, quality of life, and health resources utilization in patients with major depressive disorder seeking primary health care in Spain. Prim Care Companion J Clin Psychiatry 10(5):355–362
Ormel J, Oldehinkel A, Nolen W et al (2004) Psychosocial disability before, during, and after a major depressive episode: a 3-wave population-based study of state, scar and trait effects. Arch Gen Psychiatry 61:387–392
Ormel J, Von Korff M, Van den Brink W et al (1993) Depression, anxiety, and social disability show synchrony of change in primary care patients. Am J Public Health 83(3):385–390
Acknowledgments
We are grateful to all patients for their time and effort. We thank the University Medical Center Utrecht Primary Care Network and its participating general practitioners for participation in this study. Mirjam Geerlings had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The study was funded by European Commission’s Fifth Framework (Grant number PREDICT-QL4-CT2002-00683) and a VIDI grant from the Netherlands Organization for Scientific Research (NWO Project number 917-66-311). The funding sources had no further role in study design, in the collection, analysis and interpretation of data, in the writing of the report, and in the decision to submit the paper for publication.
Conflict of interest
All authors report no conflicts of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Stegenga, B.T., Kamphuis, M.H., King, M. et al. The natural course and outcome of major depressive disorder in primary care: the PREDICT-NL study. Soc Psychiatry Psychiatr Epidemiol 47, 87–95 (2012). https://doi.org/10.1007/s00127-010-0317-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-010-0317-9