Abstract
Objectives
The objective of this paper was to describe primary care prescribers’ perspectives on electronic prescribing drug alerts at the point of prescribing.
Design
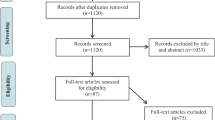
We used a mixed-method study which included clinician surveys (web-based and paper) and focus groups with prescribers and staff.
Participants
Prescribers (n = 157) working in one of 64 practices using 1 of 6 e-prescribing technologies in 6 US states completed the quantitative survey and 276 prescribers and staff participated in focus groups.
Measurements
The study measures self-reported frequency of overriding of drug alerts; open-ended responses to: “What do you think of the drug alerts your software generates for you?”
Results
More than 40% of prescribers indicated they override drug–drug interactions most of the time or always (range by e-prescribing system, 25% to 50%). Participants indicated that the software and the interaction alerts were beneficial to patient safety and valued seeing drug–drug interactions for medications prescribed by others. However, they noted that alerts are too sensitive and often unnecessary. Participant suggestions included: (1) run drug alerts on an active medication list and (2) allow prescribers to set the threshold for severity of alerts.
Conclusions
Primary care prescribers recognize the patient safety value of drug prescribing alerts embedded within electronic prescribing software. Improvements to increase specificity and reduce alert overload are needed.

Similar content being viewed by others
References
Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348:1556–64.
Gurwitz JH, Field TS, Harrold L, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289:1107–16.
Field TS, Gilman BH, Subramanian S, Fuller JC, Bates DW, Gurwitz JH. The costs associated with adverse drug events among older adults in the ambulatory setting. Med Care. 2005;43(12):1171–6.
Corley ST. Electronic prescribing: A review of costs and benefits. Top Health Inform Manage. 2003;24(1):29–38.
van der Sijs H, Aarts J, Vulto A, Berg M. Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006;13(2):138–47.
Shah N, Seger AC, Seger DL, et al. Improving acceptance of computerized prescribing alerts in ambulatory care. J Am Med Inform Assoc. 2006;13(1):5–11.
Avery AJ, Savelyich BS, Sheikh A, Morris CJ, Bowler I, Teasdale S. Improving general practice computer systems for patient safety: qualitative study of key stakeholders. Qual Saf Health Care. 2007;16(1):28–33.
Tamblyn R, Huang A, Perreault R, et al. The medical office of the 21st century (MOXXI): effectiveness of computerized decision-making support in reducing inappropriate prescribing in primary care. CMAJ. 2003;169(6):549–56.
Agresti A. Categorical data analysis: 2nd edition. New York: Wiley-Interscience; 2002.
Bell DS, Cretin S, Marken RS, Landman AB. A conceptual framework for evaluating outpatient electronic prescribing systems based on their functional capabilities. J Am Med Inform Assoc. 2004;11:60–70.
Spina J, Glassman PA, Belperio P, Cader R, Asch S. Primary Care Investigative Group of the VA Los Angeles Healthcare System. Clinical relevance of automated drug alerts from the perspective of medical providers. Am J Med Qual. 2005;20(1):7–14.
National Association of Boards of Pharmacy. Information packet: Omnibus Budget Reconciliation counseling and drug use review requirements. Park Ridge, IL, Publ. no. 101-508. 104 Stat 1388, 4401 (February, 1992).
Smith DH, Perrin N, Feldstein A, et al. The impact of prescribing safety alerts for elderly persons in an electronic medical record: an interrupted time series evaluation. Arch Intern Med. 2006;166(10):1098–104.
Weingart SN, Toth M, Sands DZ, Aronson MD, Davis RB, Phillips RS. Physicians’ decisions to override computerized drug alerts in primary care. Arch Intern Med. 2003;163(21):2625–31.
Foxhall K. E-prescribing goes to Washington. With the federal government behind it, fselectronic prescribing is gaining speed, weight, and more standards. Healthc Inform. 2007;24(6):14–5.
Tamblyn R, Huang A, Kawasumi Y, et al. The development and evaluation of an integrated electronic prescribing and drug management system for primary care. J Am Med Inform Assoc. 2006;13(2):148–59.
Bell DS, Friedman MA. E-prescribing and the Medicare Modernization Act of 2003. Health Aff. (Millwood). 2005;24(5):1159–69.
Acknowledgments
We gratefully acknowledge the assistance of Ken Whittemore, RPh, MBA and Ajit Dhalve, PharmD, MBA, of SureScripts in facilitating access to the software vendors and physician practices. This research was funded by a cooperative agreement entitled “Maximizing effectiveness of e-prescribing between physicians and community pharmacies” from AHRQ (U18 HS016394-01) to SureScripts. Mr. Whittemore and Dr. Dhalve did not participate in the collection, analysis, or interpretation of these data.
Conflict of Interest
A grant entitled “Maximizing effectiveness of e-prescribing between physicians and community pharmacies” funded by Agency for Healthcare Research and Quality Collaborative Agreement U18 HS016394-01 supported this research. Dr. Lapane [although not affiliated with SureScripts in any way (financial or otherwise)] was the principal investigator on the AHRQ-funded project. As a result, Brown University received a subcontract from SureScripts to conduct the evaluation of the AHRQ-funded project, funding for a graduate student to complete the final report to AHRQ, and funds to pay for the costs associated with performing a patient survey which were not allowable expenses on the AHRQ grant. None of the authors have any financial relationships with any of the vendors participating in this study. The authors have no other conflicts to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lapane, K.L., Waring, M.E., Schneider, K.L. et al. A Mixed Method Study of the Merits of E-Prescribing Drug Alerts in Primary Care. J GEN INTERN MED 23, 442–446 (2008). https://doi.org/10.1007/s11606-008-0505-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-008-0505-4