Abstract
Background
Comorbidity—a condition that co-exists with a primary illness—is common among older persons with heart failure and can complicate the overall management of this population.
Objectives
To determine the relationship between advancing age and the prevalence and patterns of comorbidity among older persons with heart failure.
Design
Retrospective longitudinal cohort study
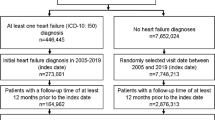
Participants
A total of 201,130 Medicare beneficiaries with heart failure stratified into three age strata in 2001: 66–75, 76–85, and 86+ years, and followed over 5 years.
Measurements
(1) Prevalence of 19 conditions as identified by the Chronic Conditions Warehouse from Medicare claims data, characterized as concordant (related to heart failure) or discordant (unrelated to heart failure), and (2) overall comorbidity burden, defined as count of conditions.
Results
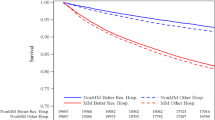
The median number of comorbidities rose from four (IQR: 2–5) to five (IQR: 4–7) among the young-old, and from 4 (IQR: 3–6) to 6 (IQR: 5–8) among the middle-old and oldest-old between 2001 and 2006. In 2001, the majority of concordant conditions were more prevalent among the youngest than oldest beneficiaries (e.g., diabetes 46.2% vs 26.9%; kidney disease 21.8% vs 18.4%), while the majority of discordant conditions were more prevalent among the oldest-old than youngest-old beneficiaries (e.g., dementia 39.6% vs 9.9%; hip fracture 9.5% vs 1.9%). Discordant conditions increased in prevalence faster among the oldest than youngest beneficiaries (e.g., dementia 13% points versus 9% points).
Conclusion
Among older Medicare beneficiaries with heart failure, there is a higher overall burden of comorbidity and greater prevalence of discordant comorbidity among the oldest old. Comorbidity prevalence increases over time, with discordant comorbidity increasing at the fastest rate among the oldest old. This comorbidity burden highlights the challenge of effectively treating heart failure while simultaneously managing co-existing and unrelated conditions.




Similar content being viewed by others
References
Lang CC, Mancini DM. Non-cardiac comorbidities in chronic heart failure. Heart. 2007;93:665–71.
Walke LM, Byers AL, Tinetti ME, Dubin JA, McCorkle R, Fried TR. Range and severity of symptoms over time among older adults with chronic obstructive pulmonary disease and heart failure. Arch Intern Med. 2007;167:2503–8.
Masoudi FA, Krumholz HM. Polypharmacy and comorbidity in heart failure. BMJ. 2003;327:513–4.
Tsuchihashi M, Tsutsui H, Kodama K, et al. Medical and socioenvironmental predictors of hospital readmission in patients with congestive heart failure. Am Heart J. 2001;142:E7.
Krumholz HM, Chen YT, Wang Y, Vaccarino V, Radford MJ, Horwitz RI. Predictors of readmission among elderly survivors of admission with heart failure. Am Heart J. 2000;139:72–7.
Bruch C, Rothenburger M, Gotzmann M, et al. Chronic kidney disease in patients with chronic heart failure–impact on intracardiac conduction, diastolic function and prognosis. Int J Cardiol. 2007;118:375–80.
Rusinaru D, Saaidi I, Godard S, Mahjoub H, Battle C, Tribouilloy C. Impact of chronic obstructive pulmonary disease on long-term outcome of patients hospitalized for heart failure. Am J Cardiol. 2008;101:353–8.
From AM, Leibson CL, Bursi F, et al. Diabetes in heart failure: prevalence and impact on outcome in the population. Am J Med. 2006;119:591–9.
Braunstein JB, Anderson GF, Gerstenblith G, et al. Noncardiac comorbidity increases preventable hospitalizations and mortality among Medicare beneficiaries with chronic heart failure. J Am Coll Cardiol. 2003;42:1226–33.
Go AS, Yang J, Ackerson LM, et al. Hemoglobin level, chronic kidney disease, and the risks of death and hospitalization in adults with chronic heart failure: the Anemia in Chronic Heart Failure: Outcomes and Resource Utilization (ANCHOR) Study. Circulation. 2006;113:2713–23.
Marengoni A, Rizzuto D, Wang HX, Winblad B, Fratiglioni L. Patterns of chronic multimorbidity in the elderly population. J Am Geriatr Soc. 2009;57:225–30.
Senni M, Santilli G, Parrella P, et al. A novel prognostic index to determine the impact of cardiac conditions and co-morbidities on one-year outcome in patients with heart failure. Am J Cardiol. 2006;98:1076–82.
Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–76.
Marengoni A, Winblad B, Karp A, Fratiglioni L. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am J Public Health. 2008;98:1198–200.
Lee SJ, Go A, Lindquist K, Bertenthal D, Covinsky KE. Chronic conditions and mortality among the oldest old. AJPH. 2008;98:1209–1214.
Corrada MM, Brookmeyer R, Paganini-Hill A, Berlau D, Kawas CH. Dementia incidence continues to increase with age in the oldest old: the 90+ study. Ann Neurol. 2010;67:114–21.
Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29:725–31.
Sales AE, Tipton EF, Levine DA, et al. Are co-morbidities associated with guideline adherence? The MI-Plus study of Medicare patients. J Gen Intern Med. 2009;24:1205–10.
Schneider KM, O'Donnell BE, Dean D. Prevalence of multiple chronic conditions in the United States' Medicare population. Health Qual Life Outcomes. 2009;7:82.
Havranek EP, Masoudi FA, Westfall KA, Wolfe P, Ordin DL, Krumholz HM. Spectrum of heart failure in older patients: results from the National Heart Failure Project. Am Heart J. 2001;143:412–7.
Senni M, Tribouilloy C, Rodeheffer RJ, et al. Congestive heart failure in the community: a study of all incident cases in Olmsted County, Minnesota, in 1991. Circulation. 1998;98:2282–9.
Goldberg RJ, Ciampa J, Lessard D, Meyer TE, Spencer FA. Long-term survival after heart failure: a contemporary population-based perspective. Arch Intern Med. 2007;167:490–6.
Curtis LH, Greiner MA, Hammill BG, et al. Early and long-term outcomes of heart failure in elderly persons, 2001–2005. Arch Intern Med. 2008;168:2481–8.
The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325:293–302.
The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II). Lancet. 1999;353:9–13.
Swedberg K, Kjekshus J. Effects of enalapril on mortality in severe congestive heart failure: results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). Am J Cardiol. 1988;62:60A–66A.
Cohn JN, Johnson G, Ziesche S, et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med. 1991;325:303–10.
Packer M, Bristow MR, Cohn JN, et al. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. US Carvedilol Heart Failure Study Group. N Engl J Med. 1996;334:1349–55.
Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999;353:2001–7
Hunt SA, Abraham WT, Chin MH, et al. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112:e154–235.
Jessup M, Abraham WT, Casey DE, et al. 2009 focused update: ACCF/AHA Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:1977–2016.
Kannel WB, Hjortland M, Castelli WP. Role of diabetes in congestive heart failure: the Framingham study. Am J Cardiol. 1974;34:29–34.
Suwanno J, Petpichetchian W, Riegel B, Issaramalai SA. A model predicting health status of patients with heart failure. J Cardiovasc Nurs. 2009;24:118–26.
Blinderman CD, Homel P, Billings JA, Portenoy RK, Tennstedt SL. Symptom distress and quality of life in patients with advanced congestive heart failure. J Pain Symptom Manage. 2008;35:594–603.
Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases. N Engl J Med. 1998;338:1516–20.
Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA. 2005;294:716–24.
Cleland JG, Clark AL. Delivering the cumulative benefits of triple therapy to improve outcomes in heart failure: too many cooks will spoil the broth. J Am Coll Cardiol. 2003;42:1234–7.
Klabunde CN, Warren JL, Legler JM. Assessing comorbidity using claims data: an overview. Med Care. 2002;40(IV):26–35.
Bursi F, Weston SA, Redfield MM, et al. Systolic and diastolic heart failure in the community. Jama. 2006;296:2209–16.
Ilksoy N, Hoffman M, Moore RH, Easley K, Jacobson TA. Comparison of African-American patients with systolic heart failure versus preserved ejection fraction. Am J Cardiol. 2006;98:806–8.
Zile MR, Brutsaert DL. New concepts in diastolic dysfunction and diastolic heart failure: Part I: diagnosis, prognosis, and measurements of diastolic function. Circulation. 2002;105:1387–93.
Acknowledgements
Dr. Ahluwalia was supported by a training grant from the National Institute on Aging (T32AG1934) and is currently supported by an Office of Academic Affiliation’s VA Associated Health Postdoctoral Fellowship Program at the VA Greater Los Angeles HSR&D Center of Excellence. Dr. Fried is a recipient of a Midcareer Investigator Award in Patient-Oriented Research from the National Institute on Aging (K24 AG028443). Dr. Chaudhry is the recipient of a Paul Beeson/K23 Career Development Award (K23AG030986) from the National Institute on Aging. Supported by the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (#2P30AG021342-06 NIH/NIA).
Presented as a poster at the 2010 Society of General Internal Medicine Annual Meeting, April 28–May 1, 2010, Minneapolis, MN.
Conflict of Interest
None disclosed
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahluwalia, S.C., Gross, C.P., Chaudhry, S.I. et al. Change in Comorbidity Prevalence with Advancing Age Among Persons with Heart Failure. J GEN INTERN MED 26, 1145–1151 (2011). https://doi.org/10.1007/s11606-011-1725-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1725-6