Abstract
BACKGROUND
Information comparing characteristics of patients who do and do not pick up their prescriptions is sparse, in part because adherence measured using pharmacy claims databases does not include information on patients who never pick up their first prescription, that is, patients with primary non-adherence. Electronic health record medication order entry enhances the potential to identify patients with primary non-adherence, and in organizations with medication order entry and pharmacy information systems, orders can be linked to dispensings to identify primarily non-adherent patients.
OBJECTIVE
This study aims to use database information from an integrated system to compare patient, prescriber, and payment characteristics of patients with primary non-adherence and patients with ongoing dispensings of newly initiated medications for hypertension, diabetes, and/or hyperlipidemia.
DESIGN
This is a retrospective observational cohort study.
PARTICIPANTS (OR PATIENTS OR SUBJECTS)
Participants of this study include patients with a newly initiated order for an antihypertensive, antidiabetic, and/or antihyperlipidemic within an 18-month period.
MAIN MEASURES
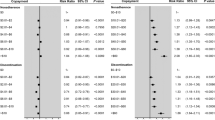
Proportion of patients with primary non-adherence overall and by therapeutic class subgroup. Multivariable logistic regression modeling was used to investigate characteristics associated with primary non-adherence relative to ongoing dispensings.
KEY RESULTS
The proportion of primarily non-adherent patients varied by therapeutic class, including 7% of patients ordered an antihypertensive, 11% ordered an antidiabetic, 13% ordered an antihyperlipidemic, and 5% ordered medications from more than one of these therapeutic classes within the study period. Characteristics of patients with primary non-adherence varied across therapeutic classes, but these characteristics had poor ability to explain or predict primary non-adherence (models c-statistics = 0.61–0.63).
CONCLUSIONS
Primary non-adherence varies by therapeutic class. Healthcare delivery systems should pursue linking medication orders with dispensings to identify primarily non-adherent patients. We encourage conduct of research to determine interventions successful at decreasing primary non-adherence, as characteristics available from databases provide little assistance in predicting primary non-adherence.

Similar content being viewed by others
References
Balkrishnan R. The importance of medication adherence in improving chronic-disease related outcomes: what we know and what we need to further know. Med Care. 2005;43:517–20.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97.
Walker EA, Molitch M, Kramer MK, et al. Adherence to preventive medications: predictors and outcomes in the Diabetes Prevention Program. Diabetes Care. 2006;29:1997–2002.
Wu JR, Moser DK, DeJong MJ, et al. Defining an evidence-based cutpoint for medication adherence in heart failure. Am Heart J. 2009;157:285–91.
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–30.
Ho PM, Magid DJ, Shetterly SM, et al. Importance of therapy intensification and medication nonadherence for blood pressure control in patients with coronary disease. Arch Intern Med. 2008;168:271–6.
McGinnis BD, Olson KL, Delate TMA, Stolcpart RS. Statin adherence and mortality in patients enrolled in a secondary prevention program. Am J Manag Care. 2009;15:689–95.
Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–41.
Andrade SE, Kahler KH, Frech F, Chan KA. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15:565–74.
Shah NR, Hirsch AG, Zacker C, Taylor S, Wood GC, Stewart WF. Factors associated with first-fill adherence rates for diabetic medications: a cohort study. J Gen Intern Med. 2009;24:233–7.
Beardon PHG, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM. Primary non-compliance with prescribed medication. Br Med J. 1993;307:846–68.
Karter AJ, Parker MM, Moffet HH, Ahmed AM, Schmittdiel JA, Selby JV. New prescription medication gaps: a comprehensive measure of adherence to new prescriptions. Health Serv Res. 2009;44(5p1):1640–61.
Shah NR, Hirsch AG, Zacker C, et al. Predictors of first-fill adherence for patients with hypertension. Am J Hypertens. 2009;22:392–6.
Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25:284–90.
Carroll NM, Ellis JL, Luckett C, Raebel MA. Feasibility of determining medication adherence from electronic health record medications orders. J Am Med Inform Assoc 2011, doi:10.1136/amiajnl-2011-000151
Hess LM, Raebel MA, Conner DA, Malone DC. Measurement of adherence in pharmacy administrative databases: a proposal for standard definitions and preferred measures. Ann Pharmacother. 2006;40:1280–8.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-Cm and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Karter AJ, Parker MM, Adams AS, et al. Primary non-adherence to prescribed medications. J Gen Intern Med. 2010;25:763.
Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. Adherence to cardiovascular disease medications: does patient-provider race/ethnicity and language concordance matter? J Gen Intern Med. 2010;25:1172–7.
Batal HA, Krantz MJ, Dale RA, Mehler PS, Steiner JF. Impact of prescription size on statin adherence and cholesterol levels. BMG Health Serv Res. 2007;7:175.
Kripalani S, Gatti ME, Jacobson TA. Association of age, health literacy, and medication management strategies with cardiovascular medication adherence. Patient Educ Couns. 2010;178(81):177–81.
Mann DM, Woodward M, Munter P, Falzon L, Kronish I. Predictors of nonadherence to statins: a systematic review and meta-analysis. Ann Pharmacother. 2010;44:1410–21.
Colombi AM, Yu-Isenberg K, Priest J. The effects of health plan copayments on adherence to oral diabetes medication and health resource utilization. J Occup Environ Med. 2008;50:535–41.
Briesacher BA, Andrade SE, Fouayzi H, Chan KA. Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacother. 2008;28:437–43.
Mann DM, Allengrante JP, Natarajan S, et al. Predictors of adherence to statins for primary prevention. Cardiovasc Drugs Ther. 2007;21:311–6.
Haskard Zolnierek HB, DiMatteo MR. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–34.
Kalsekar ID, Madhaven SS, Amonkar MM, et al. Depression in patients with type 2 diabetes: impact on adherence to oral hypoglycemic agents. Ann Pharmacother. 2006;40:605–11.
Mateo JF, Gil-Guillen VF, Mateo E, Orozco D, Carbayo JA, Merino J. Multifactorial approach and adherence to prescribed oral medications in patients with type 2 diabetes. Int J Clin Pract. 2006;60:422–8.
Tseng CW, Tierney EF, Gerzoff RB, et al. Race/ethnicity and economic differences in cost-related medication underuse among insured adults with diabetes. Diabetes Care. 2008;31:261–6.
Chan DC, Shrank WH, Cutler D, et al. Patient, physician, and payment predictors of statin adherence. Med Care. 2010;48:196–202.
Fung V, Sinclair F, Wang H, Dailey D, Hsu J, Shaber R. Patients' perspectives on nonadherence to statin therapy: a focus-group study. Permanente J. 2010;14:4–10.
Olson KL, Rasmussen J, Sandhoff BG, Merenich JA, for the Clinical Pharmacy Cardiac Risk Service (CPCRS) Study Group. Lipid management in patients with coronary artery disease by a clinical pharmacy service in a group model health maintenance organization. Arch Intern Med. 2005;165:49–54.
Merenich JA, Olson KL, Delate T, et al. Mortality reduction benefits of a comprehensive cardiac care program for patients with occlusive coronary artery disease. Pharmacother. 2007;27:1370–8.
Steiner JF, Ho PM, Beaty BL, et al. Sociodemographic and clinical characteristics are not clinically useful predictors of refill adherence in patients with hypertension. Circulation: Cardiovasc Qual Outcomes. 2010;2:452–7.
Steiner JS. Can we identify clinical predictors of medication adherence … and should we? Med Care. 2010;48:193–5.
Acknowledgments
We thank Capp Luckett for programming efforts. This study was supported by an internal grant from Kaiser Permanente Colorado. Dr. Schroeder is also supported by Training Grant 5 T32 DK007446 from the National Institute of Diabetes and Digestive and Kidney Diseases.
Conflict of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raebel, M.A., Ellis, J.L., Carroll, N.M. et al. Characteristics of Patients with Primary Non-adherence to Medications for Hypertension, Diabetes, and Lipid Disorders. J GEN INTERN MED 27, 57–64 (2012). https://doi.org/10.1007/s11606-011-1829-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-011-1829-z