ABSTRACT
BACKGROUND
Potentially teratogenic medications are frequently prescribed without provision of contraceptive counseling.
OBJECTIVE
To evaluate whether computerized clinical decision support (CDS) can increase primary care providers’ (PCPs’) provision of family planning services when prescribing potentially teratogenic medications.
DESIGN
Cluster-randomized trial conducted in one academic and one community-based practice between October of 2008 and April of 2010.
PARTICIPANTS/INTERVENTIONS
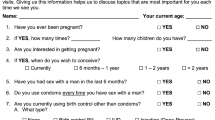
Forty-one PCPs were randomized to receive one of two types of CDS which alerted them to risks of medication-induced birth defects when ordering potentially teratogenic medications for women who may become pregnant. The ‘simple’ CDS provided a cautionary alert; the ‘multifaceted’ CDS provided tailored information and links to a structured order set designed to facilitate safe prescribing. Both CDS systems alerted PCPs about medication risk only once per encounter.
MAIN MEASURES
We assessed change in documented provision of family planning services using data from 35,110 encounters and mixed-effects models. PCPs completed surveys before and after the CDS systems were implemented, allowing assessment of change in PCP-reported counseling about the risks of medication-induced birth defects and contraception.
KEY RESULTS
Both CDS systems were associated with slight increases in provision of family planning services when potential teratogens were prescribed, without a significant difference in improvement by CDS complexity (p = 0.87). Because CDS was not repeated, 13% of the times that PCPs received CDS they substituted another potential teratogen. PCPs reported significant improvements in several counseling and prescribing practices. The multifaceted group reported a greater increase in the number of times per month they discussed the risks of medication use during pregnancy (multifaceted: +4.9 ± 7.0 vs. simple: +0.8 ± 3.2, p = 0.03). The simple CDS system was associated with greater clinician satisfaction.
CONCLUSIONS
CDS systems hold promise for increasing provision of family planning services when fertile women are prescribed potentially teratogenic medications, but further refinement of these systems is needed.


Similar content being viewed by others
References
Schwarz EB, Maselli J, Norton M, Gonzales R. Prescription of teratogenic medications in United States ambulatory practices. Am J Med. 2005;118(11):1240–9.
Schwarz EB, Postlethwaite DA, Hung YY, Armstrong MA. Documentation of contraception and pregnancy when prescribing potentially teratogenic medications for reproductive-age women. Ann Intern Med. 2007;147(6):370–6.
Santucci AK, Gold MA, Akers AY, Borrero S, Schwarz EB. Women's perspectives on counseling about risks for medication-induced birth defects. Birth Defects Res A Clin Mol Teratol. 2010;88(1):64–9.
Nordeng H, Koren G, Einarson A. Pregnant women's beliefs about medications–a study among 866 Norwegian women. Ann Pharmacother. 2010;44(9):1478–84.
Andrade SE, Gurwitz JH, Davis RL, et al. Prescription drug use in pregnancy. Am J Obstet Gynecol. 2004;191(2):398–407.
Lee E, Maneno MK, Smith L, et al. National patterns of medication use during pregnancy. Pharmacoepidemiol Drug Saf. 2006;15(8):537–45.
Sanz E, Gomez-Lopez T, Martinez-Quintas MJ. Perception of teratogenic risk of common medicines. Eur J Obstet Gynecol Reprod Biol. 2001;95(1):127–31.
Pole M, Einarson A, Pairaudeau N, Einarson T, Koren G. Drug labeling and risk perceptions of teratogenicity: A survey of pregnant Canadian women and their health professionals. J Clin Pharmacol. 2000;40(6):573–7.
Bankole A, Singh S, Haas T. Reasons why women have induced abortions: Evidence from 27 countries. International Fam Plann Perspect. 1998;24(3):117-27, 152.
Akers AY, Gold MA, Borrero S, Santucci A, Schwarz EB. Providers' perspectives on challenges to contraceptive counseling in primary care settings. J Womens Health (Larchmt). 2010;19(6):1163–70.
Schwarz EB, Santucci A, Borrero S, Akers AY, Nikolajski C, Gold MA. Perspectives of primary care clinicians on teratogenic risk counseling. Birth Defects Res A Clin Mol Teratol. 2009;85(10):858–63.
Schedlbauer A, Prasad V, Mulvaney C, et al. What evidence supports the use of computerized alerts and prompts to improve clinicians' prescribing behavior? J Am Med Inform Assoc. 2009;16(4):531–8.
Wipfli R, Lovis C. Alerts in clinical information systems: Building frameworks and prototypes. Stud Health Technol Inform. 2010;155:163–9.
Raebel MA, Carroll NM, Kelleher JA, Chester EA, Berga S, Magid DJ. Randomized trial to improve prescribing safety during pregnancy. J Am Med Inform Assoc. 2007;14(4):440–50.
Murray DM. Design and analysis of group-randomized trials. New York: Oxford University Press; 1998.
Raudenbush SW, Bryk AS. Hierarchal linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage Publications; 2002.
Schwarz EB, Longo LS, Zhao X, Stone RA, Cunningham F, Good CB. Provision of potentially teratogenic medications to female veterans of childbearing age. Med Care. 2010;48(9):834–42.
Hillemeier MM, Weisman CS, Chase GA, Dyer AM, Shaffer ML. Women's preconceptional health and use of health services: Implications for preconception care. Health Serv Res. 2008;43(1 Pt 1):54–75.
Schreiber CA, Harwood BJ, Switzer GE, Creinin MD, Reeves MF, Ness RB. Training and attitudes about contraceptive management across primary care specialties: A survey of graduating residents. Contraception. 2006;73(6):618–22.
Spencer AL, Kern LM. Primary care program directors' perceptions of women's health education: A gap in graduate medical education persists. J Womens Health (Larchmt). 2008;17(4):549–56.
Parisi SM, Zikovich S, Chuang CH, Sobota M, Nothnagle M, Schwarz EB. Primary care physicians’ perceptions of rates of unintended pregnancy. Contraception. Epub 2011 Dec 14 [doi: 10.1016/j.contraception.2011.11.004].
Henderson JT, Weisman CS, Grason H. Are two doctors better than one? Women's physician use and appropriate care. Womens Health Issues. 2002;12(3):138–49.
Gilchrist VJ, Stange KC, Flocke SA, McCord G, Bourget CC. A comparison of the National Ambulatory Medical Care Survey (NAMCS) measurement approach with direct observation of outpatient visits. Med Care. 2004;42:276–80.
Lee JK, Parisi SM, Akers AY, Borrero S, Schwarz EB. The impact of contraceptive counseling in primary care on contraceptive use. J Gen Intern Med. 2011;26(7):731–6.
ACKNOWLEDGEMENTS
This investigator-initiated study was funded by the Agency for Healthcare Research and Quality (AHRQ R18HS017093). Further support was received from NICHD K23 funds (Dr. Schwarz) and grants from the NIH and The Roadmap/NCRR/University of Pittsburgh Multidisciplinary Clinical Research Career Development Award (Dr. Handler). Many thanks to Wishwa Kapoor, MD, MPH for help with project implementation and Doug Landsittel, PhD for statistical guidance. An abstract on the physician survey data was presented at the AHRQ Health IT grantee meeting, Washington DC, June 2, 2010. An abstract on the EMR data was presented at the 1st European Congress on Preconception Care and Health, Brussels, Belgium, October 8, 2010. This work was also presented at the Epic Users’ Group Meeting, Madison, Wisconsin, September 21, 2011.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial Registration
ClinicalTrials.gov Identifier: NCT00766207
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 171 kb)
Rights and permissions
About this article
Cite this article
Schwarz, E.B., Parisi, S.M., Handler, S.M. et al. Clinical Decision Support to Promote Safe Prescribing to Women of Reproductive Age: A Cluster-Randomized Trial. J GEN INTERN MED 27, 831–838 (2012). https://doi.org/10.1007/s11606-012-1991-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-1991-y