ABSTRACT
BACKGROUND
Obesity is a stigmatizing condition associated with adverse psychosocial consequences. The relative importance of weight stigma in reducing health utility or the value a person places on their current health state is unknown.
METHODS
We conducted a telephone survey of patients with obesity. All were seeking weight loss surgery at two bariatric centers (70 % response rate). We assessed patients’ health utility (preference-based quality life measure) via a series of standard gamble scenarios assessing patients’ willingness to risk death to lose various amounts of weight or achieve perfect health (range 0 to 1; 0 = death and 1 = most valued health/weight state). Multivariable models assessed associations among quality of life domains from the Short-form 36 (SF-36) and Impact of Weight on Quality of Life-lite (IWQOL-lite) and patients’ health utility.
RESULTS
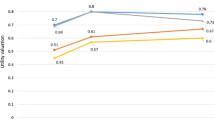
Our study sample (n = 574) had a mean body mass index of 46.5 kg/m2 and a mean health utility of 0.87, reflecting the group’s average willingness to accept a 13 % risk of death to achieve their most desired health/weight state; utilities were highly variable, however, with 10 % reporting a utility of 1.00 and 27 % reporting a utility lower than 0.90. Among the IWQOL-lite subscales, Public Distress and Work Life were the only two subscales significantly associated with patients’ utility after adjustment for sociodemographic factors. Among the SF-36 subscales, Role Physical, Physical Functioning, and Role Emotional were significantly associated with patients’ utility. When the leading subscales on both IWQOL-lite and SF-36 were considered together, Role Physical, Public Distress, and to a lesser degree Role Emotional remained independently associated with patients’ health utility.
CONCLUSION
Patients seeking weight loss surgery report health utilities similar to those reported for people living with diabetes or with laryngeal cancer; however, utility values varied widely with more than a quarter of patients willing to accept more than a 10 % risk of death to achieve their most valued health/weight state. Interference with role functioning due to physical limitations and obesity-related social stigma were strong determinants of reduced health utility.



Similar content being viewed by others
REFERENCES
Flegal KM, et al. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–41.
Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S.
Calle EE, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of US adults. N Engl J Med. 2003;348(17):1625–38.
Resnick HE, et al. Differential effects of BMI on diabetes risk among black and white Americans. Diabetes Care. 1998;21(11):1828–35.
Stevens J. Impact of age on associations between weight and mortality. Nutr Rev. 2000;58(5):129–37.
Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788–805.
White MA, et al. Gender, race, and obesity-related quality of life at extreme levels of obesity. Obes Res. 2004;12(6):949–55.
Nguyen NT, et al. Trends in use of bariatric surgery, 2003–2008. J Am Coll Surg. 2011;213(2):261–6.
Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019–28.
Kolotkin RL, et al. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9(2):102–11.
Kolotkin RL, et al. Assessing impact of weight on quality of life. Obes Res. 1995;3(1):49–56.
Wadden TA, Phelan S. Assessment of quality of life in obese individuals. Obes Res. 2002;10(Suppl 1):50S–7.
Wee CC, Davis RB, Hamel MB. Comparing the SF-12 and SF-36 health status questionnaires in patients with and without obesity. Health Qual Life Outcomes. 2008;6:11.
Russell LB, et al. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276(14):1172–7.
Wee CC, et al. Understanding patients’ value of weight loss and expectations for bariatric surgery. Obes Surg. 2006;16(4):496–500.
Ware JE, Kosinski M, Dewey JE. How to score version two of the SF-36 health survey. QualityMetric Incorporated: 2000.
Wee CC, et al. Expectations for weight loss and willingness to accept risk among patients seeking weight loss surgery. Arch Surg. In press.
Kolotkin RL, Crosby RD. Psychometric evaluation of the impact of weight on quality of life-lite questionnaire (IWQOL-lite) in a community sample. Qual Life Res. 2002;11(2):157–71.
Corica F, et al. Construct validity of the Short Form-36 Health Survey and its relationship with BMI in obese outpatients. Obesity (Silver Spring). 2006;14(8):1429–37.
Tengs TO, Wallace A. One thousand health-related quality-of-life estimates. Med Care. 2000;38(6):583–637.
Wee CC, et al. Assessing the value of weight loss among primary care patients. J Gen Intern Med. 2004;19(12):1206–11.
Dixon S, Currie CJ, McEwan P. Utility values for obesity and preliminary analysis of the Health Outcomes Data Repository. Expert Rev Pharmacoecon Outcomes Res. 2004;4(6):657–65.
Hakim Z, Wolf A, Garrison LP. Estimating the effect of changes in body mass index on health state preferences. Pharmacoeconomics. 2002;20(6):393–404.
Groessl EJ, et al. Body mass index and quality of well-being in a community of older adults. Am J Prev Med. 2004;26(2):126–9.
Ware JE. SF-36 Health Survey. Boston, MA: Manual & Interpretaion Guide; 2002.
Kolotkin RL, et al. One-year health-related quality of life outcomes in weight loss trial participants: comparison of three measures. Health Qual Life Outcomes. 2009;7:53.
Wee CC, et al. Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann Intern Med. 2000;132(9):697–704.
Wee CC, Phillips RS, McCarthy EP. BMI and cervical cancer screening among white, African-American, and Hispanic women in the United States. Obes Res. 2005;13(7):1275–80.
Drury CA, Louis M. Exploring the association between body weight, stigma of obesity, and health care avoidance. J Am Acad Nurse Pract. 2002;14(12):554–61.
Steinbrook R. Surgery for severe obesity. N Engl J Med. 2004;350(11):1075–9.
Acknowledgments
This study was funded by the National Institute of Diabetes, Digestive and Kidney Diseases (R01 DK073302). Dr. Wee is also supported by a midcareer mentorship award from the National Institute of Health (K24DK087932). The sponsor had no role in the design or conduct of the study; the collection, management, analysis, and interpretation of the data; and the preparation, review, or approval of the manuscript. Dr. Wee conceived the research question, designed the study, obtained funding, supervised the conduct of the study, and drafted the manuscript. Drs. Jones and Wee facilitated the collection of the data. Ms. Huskey had full access to all the data, conducted all the analyses, and takes responsibility for the integrity of the data and accuracy of the data analysis. Dr. Davis provided statistical expertise and along with Drs. Hamel and Wee interpreted the data. All authors provided critical revision of the manuscript for intellectual content and approved the final manuscript. We thank the patients for participating in our study and thank the ABS study team for their efforts.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wee, C.C., Davis, R.B., Huskey, K.W. et al. Quality of Life Among Obese Patients Seeking Weight Loss Surgery: The Importance of Obesity-Related Social Stigma and Functional Status. J GEN INTERN MED 28, 231–238 (2013). https://doi.org/10.1007/s11606-012-2188-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2188-0