-
PDF
- Split View
-
Views
-
Cite
Cite
John Benson, Nicky Britten, What effects do patients feel from their antihypertensive tablets and how do they react to them? Qualitative analysis of interviews with patients, Family Practice, Volume 23, Issue 1, February 2006, Pages 80–87, https://doi.org/10.1093/fampra/cmi081
Close - Share Icon Share
Abstract
Background. Patients commonly experience palpable effects from antihypertensives. Few studies have examined patients' experiences of these effects and how they influence patients' behaviour and medicine-taking.
Objectives. To describe the palpable effects that patients attribute to their antihypertensive tablets and the ways that they react to them.
Methods. In depth interviews with a maximum variety sample of 38 patients taking antihypertensive medication in 2 mainly urban UK general practices. Qualitative analysis based upon the study's objectives.
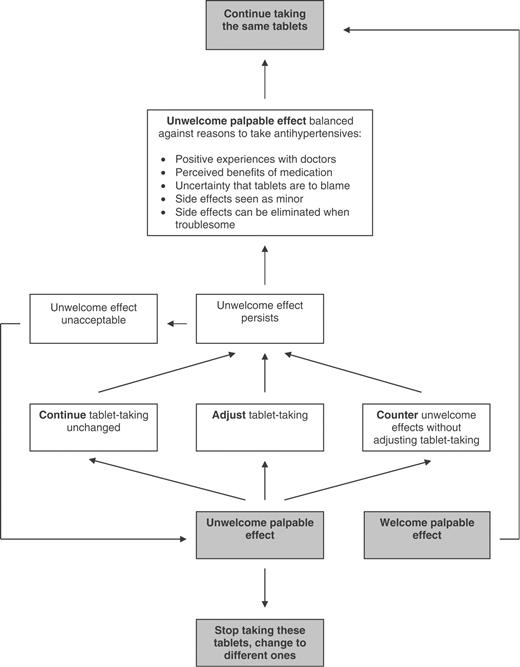
Results. Most patients attributed palpable effects to their antihypertensives. Some effects were welcome, attributed to lowered blood pressure or a calming effect of tablets, but others were unwelcome. As a result of these, some patients stopped their tablets, but more continued taking tablets as usual, took their tablets in a different way, or countered unwelcome effects by some other means. Although patients discussed stopping tablets with their doctor, they commonly did not discuss other reactions. Patients who accepted persistent unwelcome effects balanced them against reasons to take medication: positive experiences with doctors; perceived benefits of medication; or pragmatic considerations. These reasons overlap with those described previously as balancing patients' reservations about medicines.
Conclusion. The term ‘side effect’ fails to distinguish between palpable effects that are welcome or unwelcome, or to recognise that some unwelcome effects may nevertheless be acceptable. If clinicians explore the range of palpable effects that patients attribute to antihypertensives and patients' possible preparedness to tolerate unwelcome effects, they will be better able to identify patients' preferences in this area.
Benson J and Britten N. What effects do patients feel from their antihypertensive tablets and how do they react to them? Qualitative analysis of interviews with patients. Family Practice 2006; 23: 80–87.
Introduction
Side effects from antihypertensive tablets are common. In Sweden, a postal questionnaire found almost 20% of sampled antihypertensive patients reported them, whilst 26% of 1013 patients attributed at least one ‘symptom event’ to their medication in response to an open question.1,2 In separate studies, Kjellgren et al. and Morgan found that 42% and 33% of their samples of hypertensive patients had their tablets changed because of side effects.2,3 In addition, side effects have been associated with reduced medication adherence.4 Conrad found that side effects contributed to reduced medicine taking in patients with epilepsy, especially when perceived to influence social functioning5 whilst Dusing et al., surveying 11 603 patients taking antihypertensives, found that 9.6% of patients attributed reduced adherence to side effects.6 Doctors and patients may, however, use the same word but mean different things.7 They may define ‘side effects’ differently and it may be the particular meaning attached by an individual to a medication's side effects that influences their behaviour.8
In 1997–98, we undertook an interview-based study of patients' perceptions about antihypertensives. In a previously reported analysis, we found that most patients held reservations about medication but balanced these against reasons to take antihypertensives.9 So long as they take medication of any sort, patients must continue to deal with their reservations about medicines. But where side effects are both palpable and unwelcome, it is open to patients to eliminate these by changing tablets. As interviews progressed however, we noted that not only had most patients experienced unwelcome palpable effects from antihypertensives in the past, but also that many still did. Some of these patients mentioned that they had not exhausted all possible alternative tablets. We therefore conducted a qualitative analysis to explore what palpable effects patients attributed to their antihypertensives, and the consequent choices that patients made about tablet-taking.
Methods
Following local research ethics committee approval and three pilot interviews, we invited ten successive groups of patients prescribed antihypertensives in two urban practices for individual interviews exploring perceptions about their tablets. This permitted interplay between sampling, data collection and data analysis. Neither JB nor NB worked in either practice, although their patients were included in an out-of-hours rota in which JB worked. Patients were chosen to demonstrate maximum variety within theory-based categories10 derived from a literature review: age; sex; years taking antihypertensive medication; type and number of antihypertensives; numbers of non-antihypertensive medicines prescribed; and regularity of medication collection according to repeat prescription records. Where patients declined, we invited substitutes with similar characteristics. Table 1 shows the characteristics of practices and the sampling process. Table 2 shows the characteristics of interviewees.
Characteristics of practices and summary of sampling process
| Characteristic . | Practice 1 . | Practice 2 . | |
|---|---|---|---|
| Setting | Patients mainly urban, a few rural | ||
| Patient housing | Mixed: council, housing association, privately owned, rented accommodation | ||
| Patient ethnicity | Relatively low proportion of ethnic minorities | ||
| GP registrar training practice? | Yes | Yes | |
| Non trainers' patients included in study? | Yes | Yes | |
| GP whole time equivalents (WTE), n | 4.5 | 5.0 | |
| Patient registered in practices, n | 7200 | 9200 | |
| GP WTE participating in study, n | 4.5 | 3.0 | |
| Patients registered with participating GPs, n | 7200 | 5500 | |
| Patients prescribed antihypertensive medication, n | 387 | 189 | |
| Patients substituted as deemed unsuitable according to GP, n (with reason) | 3 (Dementia), 3 (Anxiety) | 1 (recent illness) | |
| Patients substituted as they did not regard themselves as taking antihypertensive medication, n | 3 | 0 | |
| Patients substituted as they declined or did not reply to invitation, n | 14 | 9 | |
| Patients interviewed, n | 29 | 9 | |
| Characteristic . | Practice 1 . | Practice 2 . | |
|---|---|---|---|
| Setting | Patients mainly urban, a few rural | ||
| Patient housing | Mixed: council, housing association, privately owned, rented accommodation | ||
| Patient ethnicity | Relatively low proportion of ethnic minorities | ||
| GP registrar training practice? | Yes | Yes | |
| Non trainers' patients included in study? | Yes | Yes | |
| GP whole time equivalents (WTE), n | 4.5 | 5.0 | |
| Patient registered in practices, n | 7200 | 9200 | |
| GP WTE participating in study, n | 4.5 | 3.0 | |
| Patients registered with participating GPs, n | 7200 | 5500 | |
| Patients prescribed antihypertensive medication, n | 387 | 189 | |
| Patients substituted as deemed unsuitable according to GP, n (with reason) | 3 (Dementia), 3 (Anxiety) | 1 (recent illness) | |
| Patients substituted as they did not regard themselves as taking antihypertensive medication, n | 3 | 0 | |
| Patients substituted as they declined or did not reply to invitation, n | 14 | 9 | |
| Patients interviewed, n | 29 | 9 | |
Characteristics of practices and summary of sampling process
| Characteristic . | Practice 1 . | Practice 2 . | |
|---|---|---|---|
| Setting | Patients mainly urban, a few rural | ||
| Patient housing | Mixed: council, housing association, privately owned, rented accommodation | ||
| Patient ethnicity | Relatively low proportion of ethnic minorities | ||
| GP registrar training practice? | Yes | Yes | |
| Non trainers' patients included in study? | Yes | Yes | |
| GP whole time equivalents (WTE), n | 4.5 | 5.0 | |
| Patient registered in practices, n | 7200 | 9200 | |
| GP WTE participating in study, n | 4.5 | 3.0 | |
| Patients registered with participating GPs, n | 7200 | 5500 | |
| Patients prescribed antihypertensive medication, n | 387 | 189 | |
| Patients substituted as deemed unsuitable according to GP, n (with reason) | 3 (Dementia), 3 (Anxiety) | 1 (recent illness) | |
| Patients substituted as they did not regard themselves as taking antihypertensive medication, n | 3 | 0 | |
| Patients substituted as they declined or did not reply to invitation, n | 14 | 9 | |
| Patients interviewed, n | 29 | 9 | |
| Characteristic . | Practice 1 . | Practice 2 . | |
|---|---|---|---|
| Setting | Patients mainly urban, a few rural | ||
| Patient housing | Mixed: council, housing association, privately owned, rented accommodation | ||
| Patient ethnicity | Relatively low proportion of ethnic minorities | ||
| GP registrar training practice? | Yes | Yes | |
| Non trainers' patients included in study? | Yes | Yes | |
| GP whole time equivalents (WTE), n | 4.5 | 5.0 | |
| Patient registered in practices, n | 7200 | 9200 | |
| GP WTE participating in study, n | 4.5 | 3.0 | |
| Patients registered with participating GPs, n | 7200 | 5500 | |
| Patients prescribed antihypertensive medication, n | 387 | 189 | |
| Patients substituted as deemed unsuitable according to GP, n (with reason) | 3 (Dementia), 3 (Anxiety) | 1 (recent illness) | |
| Patients substituted as they did not regard themselves as taking antihypertensive medication, n | 3 | 0 | |
| Patients substituted as they declined or did not reply to invitation, n | 14 | 9 | |
| Patients interviewed, n | 29 | 9 | |
Characteristics of interviewees compared with all patients in the practices who were prescribed antihypertensive medication
| Patient characteristic . | Both practices . | Interviewees . | ||
|---|---|---|---|---|
. | n = 576 . | n = 38 . | ||
| Number of patients (% total number of patients prescribed antihypertensives) | ||||
| Age (yrs) | ||||
| <50 | 39 (7%) | 7 (18%) | ||
| 50–59 | 77 (13%) | 6 (16%) | ||
| 60–69 | 181 (31%) | 11 (29%) | ||
| 70–79 | 188 (33%) | 9 (24%) | ||
| 80+ | 89 (15%) | 5 (13%) | ||
| Sex | ||||
| Male | 220 (38%) | 20 (53%) | ||
| Female | 356 (62%) | 18 (47%) | ||
| Years taking antihypertensive medication | ||||
| 0–4 | 168 (34%) | 14 (37%) | ||
| 5–9 | 115 (20%) | 5 (13%) | ||
| 10–14 | 93 (16%) | 6 (16%) | ||
| 15–19 | 94 (16%) | 7 (18%) | ||
| 20+ | 76 (13%) | 6 (16%) | ||
| Type of antihypertensive medication | ||||
| Beta blocker | 256 (44%) | 15 (39%) | ||
| Diuretic | 302 (52%) | 17 (45%) | ||
| ACE inhibitor | 154 (27%) | 12 (32%) | ||
| Calcium antagonist | 181 (31%) | 12 (32%) | ||
| Alpha blocker | 19 (3%) | 2 (5%) | ||
| Nitrate (included as overlap of patients with CHD) | 17 (3%) | 1 (3%) | ||
| Other antihypertensive medication | 19 (3%) | 1 (3%) | ||
| Number of antihypertensives prescribed | ||||
| 1 | 282 (49%) | 19 (50%) | ||
| 2 | 225 (39%) | 15 (39%) | ||
| 3 or more | 69 (12%) | 4 (11%) | ||
| Number of non-antihypertensives prescribed | ||||
| 0 | 196 (34%) | 13 (34%) | ||
| 1 | 143 (25%) | 7 (18%) | ||
| 2 | 116 (20%) | 6 (16%) | ||
| 3 | 63 (11%) | 5 (13%) | ||
| 4 | 30 (5%) | 4 (11%) | ||
| 5 or more | 28 (5%) | 3 (8%) | ||
| Regularity of medication collection (defined as the percentage of days on which antihypertensives were available to take as prescribed according to computer records over last 3 months to 1 year. If >1 antihypertensive prescribed, lowest percentage taken) | ||||
| Data unavailable | 62 (11%) | 0 (0%) | ||
| <70% days | 42 (7%) | 5 (13%) | ||
| ≥70% <80% days | 20 (3%) | 2 (5%) | ||
| ≥80% <90% days | 64 (11%) | 3 (8%) | ||
| ≥90% <100% days | 202 (35%) | 8 (21%) | ||
| ≥100% days | 186 (32%) | 20 (53%) | ||
| Patient characteristic . | Both practices . | Interviewees . | ||
|---|---|---|---|---|
. | n = 576 . | n = 38 . | ||
| Number of patients (% total number of patients prescribed antihypertensives) | ||||
| Age (yrs) | ||||
| <50 | 39 (7%) | 7 (18%) | ||
| 50–59 | 77 (13%) | 6 (16%) | ||
| 60–69 | 181 (31%) | 11 (29%) | ||
| 70–79 | 188 (33%) | 9 (24%) | ||
| 80+ | 89 (15%) | 5 (13%) | ||
| Sex | ||||
| Male | 220 (38%) | 20 (53%) | ||
| Female | 356 (62%) | 18 (47%) | ||
| Years taking antihypertensive medication | ||||
| 0–4 | 168 (34%) | 14 (37%) | ||
| 5–9 | 115 (20%) | 5 (13%) | ||
| 10–14 | 93 (16%) | 6 (16%) | ||
| 15–19 | 94 (16%) | 7 (18%) | ||
| 20+ | 76 (13%) | 6 (16%) | ||
| Type of antihypertensive medication | ||||
| Beta blocker | 256 (44%) | 15 (39%) | ||
| Diuretic | 302 (52%) | 17 (45%) | ||
| ACE inhibitor | 154 (27%) | 12 (32%) | ||
| Calcium antagonist | 181 (31%) | 12 (32%) | ||
| Alpha blocker | 19 (3%) | 2 (5%) | ||
| Nitrate (included as overlap of patients with CHD) | 17 (3%) | 1 (3%) | ||
| Other antihypertensive medication | 19 (3%) | 1 (3%) | ||
| Number of antihypertensives prescribed | ||||
| 1 | 282 (49%) | 19 (50%) | ||
| 2 | 225 (39%) | 15 (39%) | ||
| 3 or more | 69 (12%) | 4 (11%) | ||
| Number of non-antihypertensives prescribed | ||||
| 0 | 196 (34%) | 13 (34%) | ||
| 1 | 143 (25%) | 7 (18%) | ||
| 2 | 116 (20%) | 6 (16%) | ||
| 3 | 63 (11%) | 5 (13%) | ||
| 4 | 30 (5%) | 4 (11%) | ||
| 5 or more | 28 (5%) | 3 (8%) | ||
| Regularity of medication collection (defined as the percentage of days on which antihypertensives were available to take as prescribed according to computer records over last 3 months to 1 year. If >1 antihypertensive prescribed, lowest percentage taken) | ||||
| Data unavailable | 62 (11%) | 0 (0%) | ||
| <70% days | 42 (7%) | 5 (13%) | ||
| ≥70% <80% days | 20 (3%) | 2 (5%) | ||
| ≥80% <90% days | 64 (11%) | 3 (8%) | ||
| ≥90% <100% days | 202 (35%) | 8 (21%) | ||
| ≥100% days | 186 (32%) | 20 (53%) | ||
% = percentage of column total.
Characteristics of interviewees compared with all patients in the practices who were prescribed antihypertensive medication
| Patient characteristic . | Both practices . | Interviewees . | ||
|---|---|---|---|---|
. | n = 576 . | n = 38 . | ||
| Number of patients (% total number of patients prescribed antihypertensives) | ||||
| Age (yrs) | ||||
| <50 | 39 (7%) | 7 (18%) | ||
| 50–59 | 77 (13%) | 6 (16%) | ||
| 60–69 | 181 (31%) | 11 (29%) | ||
| 70–79 | 188 (33%) | 9 (24%) | ||
| 80+ | 89 (15%) | 5 (13%) | ||
| Sex | ||||
| Male | 220 (38%) | 20 (53%) | ||
| Female | 356 (62%) | 18 (47%) | ||
| Years taking antihypertensive medication | ||||
| 0–4 | 168 (34%) | 14 (37%) | ||
| 5–9 | 115 (20%) | 5 (13%) | ||
| 10–14 | 93 (16%) | 6 (16%) | ||
| 15–19 | 94 (16%) | 7 (18%) | ||
| 20+ | 76 (13%) | 6 (16%) | ||
| Type of antihypertensive medication | ||||
| Beta blocker | 256 (44%) | 15 (39%) | ||
| Diuretic | 302 (52%) | 17 (45%) | ||
| ACE inhibitor | 154 (27%) | 12 (32%) | ||
| Calcium antagonist | 181 (31%) | 12 (32%) | ||
| Alpha blocker | 19 (3%) | 2 (5%) | ||
| Nitrate (included as overlap of patients with CHD) | 17 (3%) | 1 (3%) | ||
| Other antihypertensive medication | 19 (3%) | 1 (3%) | ||
| Number of antihypertensives prescribed | ||||
| 1 | 282 (49%) | 19 (50%) | ||
| 2 | 225 (39%) | 15 (39%) | ||
| 3 or more | 69 (12%) | 4 (11%) | ||
| Number of non-antihypertensives prescribed | ||||
| 0 | 196 (34%) | 13 (34%) | ||
| 1 | 143 (25%) | 7 (18%) | ||
| 2 | 116 (20%) | 6 (16%) | ||
| 3 | 63 (11%) | 5 (13%) | ||
| 4 | 30 (5%) | 4 (11%) | ||
| 5 or more | 28 (5%) | 3 (8%) | ||
| Regularity of medication collection (defined as the percentage of days on which antihypertensives were available to take as prescribed according to computer records over last 3 months to 1 year. If >1 antihypertensive prescribed, lowest percentage taken) | ||||
| Data unavailable | 62 (11%) | 0 (0%) | ||
| <70% days | 42 (7%) | 5 (13%) | ||
| ≥70% <80% days | 20 (3%) | 2 (5%) | ||
| ≥80% <90% days | 64 (11%) | 3 (8%) | ||
| ≥90% <100% days | 202 (35%) | 8 (21%) | ||
| ≥100% days | 186 (32%) | 20 (53%) | ||
| Patient characteristic . | Both practices . | Interviewees . | ||
|---|---|---|---|---|
. | n = 576 . | n = 38 . | ||
| Number of patients (% total number of patients prescribed antihypertensives) | ||||
| Age (yrs) | ||||
| <50 | 39 (7%) | 7 (18%) | ||
| 50–59 | 77 (13%) | 6 (16%) | ||
| 60–69 | 181 (31%) | 11 (29%) | ||
| 70–79 | 188 (33%) | 9 (24%) | ||
| 80+ | 89 (15%) | 5 (13%) | ||
| Sex | ||||
| Male | 220 (38%) | 20 (53%) | ||
| Female | 356 (62%) | 18 (47%) | ||
| Years taking antihypertensive medication | ||||
| 0–4 | 168 (34%) | 14 (37%) | ||
| 5–9 | 115 (20%) | 5 (13%) | ||
| 10–14 | 93 (16%) | 6 (16%) | ||
| 15–19 | 94 (16%) | 7 (18%) | ||
| 20+ | 76 (13%) | 6 (16%) | ||
| Type of antihypertensive medication | ||||
| Beta blocker | 256 (44%) | 15 (39%) | ||
| Diuretic | 302 (52%) | 17 (45%) | ||
| ACE inhibitor | 154 (27%) | 12 (32%) | ||
| Calcium antagonist | 181 (31%) | 12 (32%) | ||
| Alpha blocker | 19 (3%) | 2 (5%) | ||
| Nitrate (included as overlap of patients with CHD) | 17 (3%) | 1 (3%) | ||
| Other antihypertensive medication | 19 (3%) | 1 (3%) | ||
| Number of antihypertensives prescribed | ||||
| 1 | 282 (49%) | 19 (50%) | ||
| 2 | 225 (39%) | 15 (39%) | ||
| 3 or more | 69 (12%) | 4 (11%) | ||
| Number of non-antihypertensives prescribed | ||||
| 0 | 196 (34%) | 13 (34%) | ||
| 1 | 143 (25%) | 7 (18%) | ||
| 2 | 116 (20%) | 6 (16%) | ||
| 3 | 63 (11%) | 5 (13%) | ||
| 4 | 30 (5%) | 4 (11%) | ||
| 5 or more | 28 (5%) | 3 (8%) | ||
| Regularity of medication collection (defined as the percentage of days on which antihypertensives were available to take as prescribed according to computer records over last 3 months to 1 year. If >1 antihypertensive prescribed, lowest percentage taken) | ||||
| Data unavailable | 62 (11%) | 0 (0%) | ||
| <70% days | 42 (7%) | 5 (13%) | ||
| ≥70% <80% days | 20 (3%) | 2 (5%) | ||
| ≥80% <90% days | 64 (11%) | 3 (8%) | ||
| ≥90% <100% days | 202 (35%) | 8 (21%) | ||
| ≥100% days | 186 (32%) | 20 (53%) | ||
% = percentage of column total.
JB conducted interviews in patients' homes using a topic guide whose content was modified during early interviews and finalised after the twelfth interview. JB introduced himself as a ‘researcher’, confirming that he was a doctor to those interviewees who asked directly. Amongst others, the topic guide asked patients the following questions about their experience of taking antihypertensives: “Is there anything you don't like about taking antihypertensive medicine?”; “what effect does/did taking the medicine have on you?”; “Good effects, not so good effects?” Where patients spoke about perceived effects, follow-up questions were asked about what they had done as a result. Interviews lasted approximately 30 minutes.
Interviews were tape-recorded with patients' consent and transcribed, labelling patients by number from 1–38. We analysed interview transcripts in five iterative steps: identification of themes; generation of a code to label transcript passages; revision of themes and coding scheme as data accumulated; code application to the final dataset; and exploration of theme relationships within and between patients.11 JB and NB generated independent initial coding schemes whose differences were resolved by discussion. JB elaborated the coding scheme and applied the final code which included patients' perceived palpable effects, the ways that patients reacted and patients' reasons for their reaction. JB and NB confirmed that the final code was consistently applied through blind dual coding of two transcripts. For each patient, we produced a coding summary sheet, identifying every code category allocated to their interview data. A line was then drawn joining code categories to indicate relationships expressed by that patient (i.e. not those inferred by the authors). We then generated a second summary sheet for each patient, generating aggregated code categories which we used to explore patterns,11 with constant reference back to the first sheet to ensure that proposed patterns remained viable at the level of the original code category. After 38 interviews (excluding pilot interviews), analysis suggested that we had reached theoretical saturation across the dataset as a whole.10 There were no systematic differences in the responses given by patients in the two practices. The validity of emergent conclusions was confirmed by respondent validation.
Results
We sent a résumé of the study's findings to all 38 interviewees, asking them to respond on a Likert scale to the statement “I feel that my views about blood pressure and blood pressure medicines can be seen in the (attached) summary” and to make free text comments should they disagree. Thirty one interviewees replied, of whom 29 (94% of respondents) agreed or agreed strongly. Two (6% of respondents) were unsure, one making no comment, the other reiterating an experience contained in their interview transcript. None disagreed or disagreed strongly.
Overall tablet-taking
Most interviewees (26 patients) mentioned sometimes missing out antihypertensives to some degree. Most felt that this happened very seldom, but some (6 patients) spoke of it happening quite often.
Some interviewees (5 patients) had made deliberate adjustments (either omissions or extra doses).Interviewee 25 “I very easily forget them. I have a routine in the morning which is a glass of orange juice, take the tablet. Now if the orange juice runs out, the chances are I'll forget to take the tablet.”
Welcome effects
Patients commonly mentioned welcome effects of antihypertensives. About half of those interviewed (20 patients) said that they felt better as a result of their tablets lowering their blood pressure:
A few patients (3) mentioned a welcome calming effect from their tablets:JB “What benefits do you see as being there from taking those tablets?”
Interviewee 30 “Um, you know I don't have those sort of er, dizziness and er, and start sweating and this sort of thing, so I feel myself much more comfortable.”
Interviewee 07 “I mean, obviously, they do have their advantages because you know, like, for instance, I've had, since I became redundant, I've had six interviews. Because I've been taking timolol I've been going in as calm as anything. So they have got their advantages.”
Unwelcome effects
Rather more commonly, patients mentioned unwelcome effects. Twenty eight patients had attributed a total of 58 unwelcome effects to their antihypertensives at some point and seventeen of these patients still experienced them. The British National Formulary cites a wide range of side effects for antihypertensives, but some patients attributed effects that the formulary does not list. The following patient took a beta blocker:
Patients mentioned unwelcome effects as important factors in deciding about antihypertensives. Many patients spoke of what it would take for them to review taking their tablets and 20 mentioned unwelcome effects:Interviewee 07 “I have had … tests up the hospital for blood in my urine, which could be anything from your bladder, kidneys … but I've had them all checked out but I'm still getting the traces of blood …”
JB “Have you wondered if the blood pressure tablets were involved in that?”
Interviewee 07 “Yes, I asked the doctor and she said ‘I don't think so’. But I don't know. Obviously … that does bother me.”
Table 3 lists the range of unwelcome effects mentioned, using patients' own words. These unwelcome effects had all led patients to react in some way, sometimes more than once. About half of these reactions overall were undertaken without consulting a clinician.Interviewee 22 “… if I did get, start thinking, well they're not doing me any good, or they're affecting me in some other way, um, I'd go and tell my doctor what I was thinking.”
Unwelcome palpable effects mentioned by patients prescribed antihypertensives
| Interviewee . | Unwelcome effect . | |
|---|---|---|
| Giddiness/unsteadiness | ||
| 2 | “I felt really ill …. I just collapsed really for a few minutes” | |
| 9 | “If I get up in a hurry, I feel as if I want to sit down straight away” | |
| 13 | “It makes me all dizzy and I couldn't stand up or anything” | |
| 18 | “They sort of made my legs go sort of jellified for about an hour or so” | |
| 24 | “I collapsed at a wedding and I was in hospital” | |
| 24 | “If I stand too long that goes low and I just go down” | |
| 28 | “When I got up in the morning I was very unsteady…” | |
| 33 | “I was still feeling dizzy, I was still feeling sick” | |
| 35 | “It made me sort of feel giddy or sick…” | |
| 35 | “And I just feel for a second a little bit giddy…” | |
| Weight gain | ||
| 11 | “Only this past couple of weeks, a very big increase in weight” | |
| 26 | “I feel as though I've put on weight with them” | |
| Urinary problems | ||
| 1 | “You just go and wee quite a bit in the afternoon” | |
| 7 | “I have had to have tests up the hospital for blood in my urine” | |
| 10 | “There may be some urgency in urinating … marginal perhaps” | |
| 20 | “As soon as I got to …. I had to dive into the loo” | |
| 22 | “If we were going out shopping … then I wouldn't take a water tablet … its fatal” | |
| 27 | “Running to the loo every five minutes” | |
| 30 | “It made me wee a lot” | |
| Headache | ||
| 32 | “I had terrible headaches … I really felt a muggy head” | |
| 37 | “I used to get headaches” | |
| Tiredness | ||
| 2 | “I was so cold, so fatigued, I felt really lowly” | |
| 2 | “the atenolol was somehow fighting against the reduction of the prednisolone” | |
| 5 | “I used to feel drowsy … lackadaisical” | |
| 5 | “I can do most things now, but sometimes I get a bit weary quicker …” | |
| 7 | “I started to feel quite tired” | |
| 7 | “Once it got in my system … and I rode a bike, it was hard work” | |
| 7 | “If I went to play golf in the afternoon … I just felt like … completely drained” | |
| 14 | “Just a tiredening in the muscles” | |
| 16 | “I've been quite tired” | |
| 19 | “I felt a bit more go in me” [on changing tablets] | |
| 19 | “I get tired sometimes” | |
| 26 | “Well first of all I was very, very tired” | |
| 30 | “I found they was making me tired” | |
| Swelling | ||
| 2 | “That was the same effect as the nifedipine [swelling]” | |
| 2 | “I all swelled up, a bit like the Michelin tyre company man” | |
| 15 | “It made my ankles all swell up” | |
| 16 | “I had slightly, sort of, puffy ankles” | |
| 26 | “They make you prone to swollen ankles, which is horrible” | |
| Problems with sex | ||
| 7 | “Making love, I suppose … that does do something to your performance …” | |
| 23 | “ … quite normal apart from my sexual drive, which seems a bit down” | |
| Miscellaneous | ||
| 2 | “That caused continuous coughing and wheeziness” | |
| 2 | “I can get a mild stomach ache, probably an hour later” | |
| 4 | “Dryness in the throat … I probably thought that I might have diabetes” | |
| 15 | “If I take them in the morning they make me feel bad” | |
| 16 | “I've also had some sort of itchy rash on the shins” | |
| 16 | “Since taking the tablets there's breathlessness to a degree” | |
| 17 | “If the ringing in my ears is a side effect of the tablets, I don't know” | |
| 20 | “One of the side effects is diabetes … well I've got diabetes now, funnily enough” | |
| 23 | “Sort of feeling liverish and you can't focus properly” | |
| 24 | “I get a lot of nausea” | |
| 26 | “I got chest pains … I didn't feel quite right” | |
| 26 | “I think it's a skin condition that I've got …” | |
| 26 | “I did think, a little while ago, that it was affecting my eyesight” | |
| 32 | “ … they might be something to do with the problems with my lungs” | |
| 37 | “Just before Christmas, my foot turned blue” | |
| 38 | “At night time I get tingling in my blood” | |
| 38 | “I used to enjoy a drink but now I don't … I'm going to wake up feeling real lousy” | |
| Interviewee . | Unwelcome effect . | |
|---|---|---|
| Giddiness/unsteadiness | ||
| 2 | “I felt really ill …. I just collapsed really for a few minutes” | |
| 9 | “If I get up in a hurry, I feel as if I want to sit down straight away” | |
| 13 | “It makes me all dizzy and I couldn't stand up or anything” | |
| 18 | “They sort of made my legs go sort of jellified for about an hour or so” | |
| 24 | “I collapsed at a wedding and I was in hospital” | |
| 24 | “If I stand too long that goes low and I just go down” | |
| 28 | “When I got up in the morning I was very unsteady…” | |
| 33 | “I was still feeling dizzy, I was still feeling sick” | |
| 35 | “It made me sort of feel giddy or sick…” | |
| 35 | “And I just feel for a second a little bit giddy…” | |
| Weight gain | ||
| 11 | “Only this past couple of weeks, a very big increase in weight” | |
| 26 | “I feel as though I've put on weight with them” | |
| Urinary problems | ||
| 1 | “You just go and wee quite a bit in the afternoon” | |
| 7 | “I have had to have tests up the hospital for blood in my urine” | |
| 10 | “There may be some urgency in urinating … marginal perhaps” | |
| 20 | “As soon as I got to …. I had to dive into the loo” | |
| 22 | “If we were going out shopping … then I wouldn't take a water tablet … its fatal” | |
| 27 | “Running to the loo every five minutes” | |
| 30 | “It made me wee a lot” | |
| Headache | ||
| 32 | “I had terrible headaches … I really felt a muggy head” | |
| 37 | “I used to get headaches” | |
| Tiredness | ||
| 2 | “I was so cold, so fatigued, I felt really lowly” | |
| 2 | “the atenolol was somehow fighting against the reduction of the prednisolone” | |
| 5 | “I used to feel drowsy … lackadaisical” | |
| 5 | “I can do most things now, but sometimes I get a bit weary quicker …” | |
| 7 | “I started to feel quite tired” | |
| 7 | “Once it got in my system … and I rode a bike, it was hard work” | |
| 7 | “If I went to play golf in the afternoon … I just felt like … completely drained” | |
| 14 | “Just a tiredening in the muscles” | |
| 16 | “I've been quite tired” | |
| 19 | “I felt a bit more go in me” [on changing tablets] | |
| 19 | “I get tired sometimes” | |
| 26 | “Well first of all I was very, very tired” | |
| 30 | “I found they was making me tired” | |
| Swelling | ||
| 2 | “That was the same effect as the nifedipine [swelling]” | |
| 2 | “I all swelled up, a bit like the Michelin tyre company man” | |
| 15 | “It made my ankles all swell up” | |
| 16 | “I had slightly, sort of, puffy ankles” | |
| 26 | “They make you prone to swollen ankles, which is horrible” | |
| Problems with sex | ||
| 7 | “Making love, I suppose … that does do something to your performance …” | |
| 23 | “ … quite normal apart from my sexual drive, which seems a bit down” | |
| Miscellaneous | ||
| 2 | “That caused continuous coughing and wheeziness” | |
| 2 | “I can get a mild stomach ache, probably an hour later” | |
| 4 | “Dryness in the throat … I probably thought that I might have diabetes” | |
| 15 | “If I take them in the morning they make me feel bad” | |
| 16 | “I've also had some sort of itchy rash on the shins” | |
| 16 | “Since taking the tablets there's breathlessness to a degree” | |
| 17 | “If the ringing in my ears is a side effect of the tablets, I don't know” | |
| 20 | “One of the side effects is diabetes … well I've got diabetes now, funnily enough” | |
| 23 | “Sort of feeling liverish and you can't focus properly” | |
| 24 | “I get a lot of nausea” | |
| 26 | “I got chest pains … I didn't feel quite right” | |
| 26 | “I think it's a skin condition that I've got …” | |
| 26 | “I did think, a little while ago, that it was affecting my eyesight” | |
| 32 | “ … they might be something to do with the problems with my lungs” | |
| 37 | “Just before Christmas, my foot turned blue” | |
| 38 | “At night time I get tingling in my blood” | |
| 38 | “I used to enjoy a drink but now I don't … I'm going to wake up feeling real lousy” | |
Unwelcome palpable effects mentioned by patients prescribed antihypertensives
| Interviewee . | Unwelcome effect . | |
|---|---|---|
| Giddiness/unsteadiness | ||
| 2 | “I felt really ill …. I just collapsed really for a few minutes” | |
| 9 | “If I get up in a hurry, I feel as if I want to sit down straight away” | |
| 13 | “It makes me all dizzy and I couldn't stand up or anything” | |
| 18 | “They sort of made my legs go sort of jellified for about an hour or so” | |
| 24 | “I collapsed at a wedding and I was in hospital” | |
| 24 | “If I stand too long that goes low and I just go down” | |
| 28 | “When I got up in the morning I was very unsteady…” | |
| 33 | “I was still feeling dizzy, I was still feeling sick” | |
| 35 | “It made me sort of feel giddy or sick…” | |
| 35 | “And I just feel for a second a little bit giddy…” | |
| Weight gain | ||
| 11 | “Only this past couple of weeks, a very big increase in weight” | |
| 26 | “I feel as though I've put on weight with them” | |
| Urinary problems | ||
| 1 | “You just go and wee quite a bit in the afternoon” | |
| 7 | “I have had to have tests up the hospital for blood in my urine” | |
| 10 | “There may be some urgency in urinating … marginal perhaps” | |
| 20 | “As soon as I got to …. I had to dive into the loo” | |
| 22 | “If we were going out shopping … then I wouldn't take a water tablet … its fatal” | |
| 27 | “Running to the loo every five minutes” | |
| 30 | “It made me wee a lot” | |
| Headache | ||
| 32 | “I had terrible headaches … I really felt a muggy head” | |
| 37 | “I used to get headaches” | |
| Tiredness | ||
| 2 | “I was so cold, so fatigued, I felt really lowly” | |
| 2 | “the atenolol was somehow fighting against the reduction of the prednisolone” | |
| 5 | “I used to feel drowsy … lackadaisical” | |
| 5 | “I can do most things now, but sometimes I get a bit weary quicker …” | |
| 7 | “I started to feel quite tired” | |
| 7 | “Once it got in my system … and I rode a bike, it was hard work” | |
| 7 | “If I went to play golf in the afternoon … I just felt like … completely drained” | |
| 14 | “Just a tiredening in the muscles” | |
| 16 | “I've been quite tired” | |
| 19 | “I felt a bit more go in me” [on changing tablets] | |
| 19 | “I get tired sometimes” | |
| 26 | “Well first of all I was very, very tired” | |
| 30 | “I found they was making me tired” | |
| Swelling | ||
| 2 | “That was the same effect as the nifedipine [swelling]” | |
| 2 | “I all swelled up, a bit like the Michelin tyre company man” | |
| 15 | “It made my ankles all swell up” | |
| 16 | “I had slightly, sort of, puffy ankles” | |
| 26 | “They make you prone to swollen ankles, which is horrible” | |
| Problems with sex | ||
| 7 | “Making love, I suppose … that does do something to your performance …” | |
| 23 | “ … quite normal apart from my sexual drive, which seems a bit down” | |
| Miscellaneous | ||
| 2 | “That caused continuous coughing and wheeziness” | |
| 2 | “I can get a mild stomach ache, probably an hour later” | |
| 4 | “Dryness in the throat … I probably thought that I might have diabetes” | |
| 15 | “If I take them in the morning they make me feel bad” | |
| 16 | “I've also had some sort of itchy rash on the shins” | |
| 16 | “Since taking the tablets there's breathlessness to a degree” | |
| 17 | “If the ringing in my ears is a side effect of the tablets, I don't know” | |
| 20 | “One of the side effects is diabetes … well I've got diabetes now, funnily enough” | |
| 23 | “Sort of feeling liverish and you can't focus properly” | |
| 24 | “I get a lot of nausea” | |
| 26 | “I got chest pains … I didn't feel quite right” | |
| 26 | “I think it's a skin condition that I've got …” | |
| 26 | “I did think, a little while ago, that it was affecting my eyesight” | |
| 32 | “ … they might be something to do with the problems with my lungs” | |
| 37 | “Just before Christmas, my foot turned blue” | |
| 38 | “At night time I get tingling in my blood” | |
| 38 | “I used to enjoy a drink but now I don't … I'm going to wake up feeling real lousy” | |
| Interviewee . | Unwelcome effect . | |
|---|---|---|
| Giddiness/unsteadiness | ||
| 2 | “I felt really ill …. I just collapsed really for a few minutes” | |
| 9 | “If I get up in a hurry, I feel as if I want to sit down straight away” | |
| 13 | “It makes me all dizzy and I couldn't stand up or anything” | |
| 18 | “They sort of made my legs go sort of jellified for about an hour or so” | |
| 24 | “I collapsed at a wedding and I was in hospital” | |
| 24 | “If I stand too long that goes low and I just go down” | |
| 28 | “When I got up in the morning I was very unsteady…” | |
| 33 | “I was still feeling dizzy, I was still feeling sick” | |
| 35 | “It made me sort of feel giddy or sick…” | |
| 35 | “And I just feel for a second a little bit giddy…” | |
| Weight gain | ||
| 11 | “Only this past couple of weeks, a very big increase in weight” | |
| 26 | “I feel as though I've put on weight with them” | |
| Urinary problems | ||
| 1 | “You just go and wee quite a bit in the afternoon” | |
| 7 | “I have had to have tests up the hospital for blood in my urine” | |
| 10 | “There may be some urgency in urinating … marginal perhaps” | |
| 20 | “As soon as I got to …. I had to dive into the loo” | |
| 22 | “If we were going out shopping … then I wouldn't take a water tablet … its fatal” | |
| 27 | “Running to the loo every five minutes” | |
| 30 | “It made me wee a lot” | |
| Headache | ||
| 32 | “I had terrible headaches … I really felt a muggy head” | |
| 37 | “I used to get headaches” | |
| Tiredness | ||
| 2 | “I was so cold, so fatigued, I felt really lowly” | |
| 2 | “the atenolol was somehow fighting against the reduction of the prednisolone” | |
| 5 | “I used to feel drowsy … lackadaisical” | |
| 5 | “I can do most things now, but sometimes I get a bit weary quicker …” | |
| 7 | “I started to feel quite tired” | |
| 7 | “Once it got in my system … and I rode a bike, it was hard work” | |
| 7 | “If I went to play golf in the afternoon … I just felt like … completely drained” | |
| 14 | “Just a tiredening in the muscles” | |
| 16 | “I've been quite tired” | |
| 19 | “I felt a bit more go in me” [on changing tablets] | |
| 19 | “I get tired sometimes” | |
| 26 | “Well first of all I was very, very tired” | |
| 30 | “I found they was making me tired” | |
| Swelling | ||
| 2 | “That was the same effect as the nifedipine [swelling]” | |
| 2 | “I all swelled up, a bit like the Michelin tyre company man” | |
| 15 | “It made my ankles all swell up” | |
| 16 | “I had slightly, sort of, puffy ankles” | |
| 26 | “They make you prone to swollen ankles, which is horrible” | |
| Problems with sex | ||
| 7 | “Making love, I suppose … that does do something to your performance …” | |
| 23 | “ … quite normal apart from my sexual drive, which seems a bit down” | |
| Miscellaneous | ||
| 2 | “That caused continuous coughing and wheeziness” | |
| 2 | “I can get a mild stomach ache, probably an hour later” | |
| 4 | “Dryness in the throat … I probably thought that I might have diabetes” | |
| 15 | “If I take them in the morning they make me feel bad” | |
| 16 | “I've also had some sort of itchy rash on the shins” | |
| 16 | “Since taking the tablets there's breathlessness to a degree” | |
| 17 | “If the ringing in my ears is a side effect of the tablets, I don't know” | |
| 20 | “One of the side effects is diabetes … well I've got diabetes now, funnily enough” | |
| 23 | “Sort of feeling liverish and you can't focus properly” | |
| 24 | “I get a lot of nausea” | |
| 26 | “I got chest pains … I didn't feel quite right” | |
| 26 | “I think it's a skin condition that I've got …” | |
| 26 | “I did think, a little while ago, that it was affecting my eyesight” | |
| 32 | “ … they might be something to do with the problems with my lungs” | |
| 37 | “Just before Christmas, my foot turned blue” | |
| 38 | “At night time I get tingling in my blood” | |
| 38 | “I used to enjoy a drink but now I don't … I'm going to wake up feeling real lousy” | |
Stopping tablets or making no changes
Some patients had reacted to unwelcome effects by stopping their tablets (18 reactions). All but 2 of these effects were discussed with a doctor before stopping medication. Both of these were discussed soon afterwards.
In contrast, others continued medication unchanged despite unwelcome effects (25 reactions). Only about half of these were discussed with a doctor, patients mentioning having balanced the unwelcome effect against reasons to take antihypertensives (Fig. 1). Some balanced the unwelcome effect against positive experiences with doctors. This might involve advice from doctors or improved blood pressure readings:
Some balanced the unwelcome effect against perceived benefits of medication, either medication achieving a good outcome, or feeling better when taking it. This patient, who saw antihypertensives as protection from a heart attack spoke of both:Interviewee “… [The tablets] make you prone to swollen ankles, which is horrible, I hate it … [the doctor] is a bit reluctant to do anything really because as my blood pressure is so even on this tablet, that it might outweigh … I've talked about it and I'm thinking the same as what [the doctor] is thinking, that because my blood pressure is on an even keel I have to sort of have the good with the bad, sort of thing.”
Some patients balanced unwelcome effects against pragmatic considerations. Some were uncertain that medication was to blame:Interviewee 23 “… the erections I suppose, they don't feel so firm, you know … which is the best of the two evils, you know? I suppose I would rather take the tablets and be here, than not take them and, although, I suppose when I did have high blood pressure and had sex, I felt as though my head was banging, very, and I used to get out of breath … [now] … It's all right.”
Others saw the unwelcome effect as minor, making reaction unnecessary:Interviewee 05 “… I feel I can do most things now, but sometimes I get a bit weary quicker, mind that could be age as well couldn't it?”
Interviewee 37 “Well they weren't bad headaches and I used to think, well that's just a little side effect. It didn't bother me.”
Reactions to palpable effects and reasons for taking medication in the face of them amongst patients prescribed antihypertensives
Taking tablets differently
Some patients found a middle ground by taking their tablets in a different way (14 reactions). Similar to those continuing tablets unchanged, only about half of those who made adjustments discussed their decision with a doctor. They omitted doses or altering their timing:
Taking tablets differently did not necessarily eliminate the effect. In that case, patients either reacted a second time or accepted the effect, balancing it pragmatically against the fact that the modification eliminated the effect when it was most troublesome (Fig. 1), in this case before golf or sex:Interviewee 32 “The Cardura, that one I started taking earlier in the day and I had terrible headaches with that and so I really felt a muggy head. So they told me to take it last thing at night, so that any side effects would wear off while I'm asleep, so that in the morning I'm all right.”
Interviewee 07 “I've actually left the tablet out, um, say for instance, um, like Sunday I was playing golf in the morning, so the last one I will take would be Friday sometime, so Saturday I go completely without it … I don't get impotence, but it's the effort if you like. Because of your muscles because the adrenaline is not allowed to flow through, so you're obviously restricted. So therefore I leave it [medication] alone.”
Countering unwelcome effects
Some patients reacted by countering effects without adjusting their tablet-taking. Hardly any of these decisions were discussed with the doctor. Occasionally this eliminated the effect:
Often, the effect persisted. One patient found this persistence unacceptable and reacted a second time (see below), but the remainder balanced the continued need to make allowances for the unwelcome effect against pragmatic uncertainty that the medication was really to blame or the effect seeming only minor (Fig. 1):Interviewee 16 “I've also had some sort of itchy rashes on the sort of shins and on the sort of collar bones here, but I dose those with just ordinary hydrocortisone ointment which seems to solve the problem, so its not a massive problem.”
Interviewee 09 “… if I'm bending down outside and I get up in a hurry, I feel as if I want to sit down straight away. Not because I go dizzy, but I feel somewhat shattered and weak and then sit down and then I'm all right, so I don't bend down do I, outside too much … because it's not regular, I thought, well the next time I'm with the doctor I might just mention it, but it obviously can't be of much importance.”
Unsatisfactory outcomes and disagreement with doctors
Six reactions to an unwelcome effect did not achieve an acceptable outcome. Patients then reacted to the unwelcome effect differently. Three of these further reactions eliminated the unwelcome effect, the rest did not. Again, persistent effects were deemed acceptable through balancing them against reasons to take medication as just described.
Five patients disagreed with doctors about the significance of effects, or the reaction that should be taken. The patient who omitted medication before golf mentioned that this was not his doctor's advice and gave his reason for taking a different action:
Disagreement did not automatically lead to a different reaction to that suggested by the doctor, however. Some patients decided to follow the doctor's advice nevertheless, again rationalising their decision by balancing their reluctance to follow advice against one or more of the identified reasons to take antihypertensives (Fig. 1). Those who continued tablets on their doctor's advice might only be willing to do so after a second opinion had been obtained, however:Interviewee 07 “Once it got in my system, maybe an hour later, and I rode a bike, it was, you know, hard work … well I have told the doctors about this and they've said, why don't you take the tablet before you go to bed, which I have done, but also with the timolol, well then with all the beta-blockers, is that they calm you down. If I took it the night before, then I believe a lot of the effectiveness of the tablet's probably gone half way through the day.”
Interviewee 38 “I mean I couldn't say, well, that doctor ain't doing his job, but I thought that the tablets, the blood pressure tablet I was taking was causing, causing me a bit of trouble … the headaches and different things, so I went to see Dr [name removed], up the hospital. The wife heard about him and told me and I kept on at the doctor until I went there and yesterday I had a blood test and he said the tablets were working 100%, the blood pressure was low, so my doctor was right.”
Discussion
This study has shown that patients commonly attribute palpable effects to their antihypertensive tablets. Some of these were welcome, attributed to treatment having a beneficial effect on blood pressure related symptoms or a perception that the tablets made individuals feel calmer. Other palpable effects were unwelcome however, and although patients sometimes acted to eliminate them, that was not universal. Patients used a range of strategies to deal with unwelcome effects and, for cogent personal reasons, patients often accepted their persistence.
Strengths of the study include a diversity of participant characteristics, making these findings relevant for a wide range of antihypertensive medication users. Patients involved were, however, taking antihypertensives, so their reasoning may not be representative of those who have dropped out of treatment altogether. Alternatively, patients who drop out of treatment may do so because they are unable to reconcile unwelcome effects with reasons to take medicines. Patients identified who had dropped out of treatment declined interview, so it was impossible to explore this. A further weakness is that patients in this study were generally of white ethnicity, reflecting the population where the research was conducted. Patients of different ethnicity might behave differently.12
The term ‘side effect’ is generally taken to refer to an effect of a drug other than that for which it is administered, usually for the worse.13 The palpable effects attributed to antihypertensives by this group of patients might all be classed as side effects, especially as from a medical perspective hypertension is a generally symptomless condition.14 Where such effects were unwelcome, some patients in this study did stop taking their tablets or modified the way they took them. Svensson et al. observed that side effects or symptoms ascribed to medication were a major reason for self-reported non-adherence with antihypertensives.15 Similarly, a recent synthesis of qualitative studies examined patients' experiences of medicine taking for a variety of medical conditions. This identified adverse effects, or concern about them, as one of the factors that made patients cautious about taking medicines, leading them to experiment with reductions in dosage or periods of abstinence from taking tablets.16
Nevertheless, patients in this study did not see all palpable effects as irredeemably adverse. Some effects were welcome and for personally cogent reasons, patients tolerated many of those that were unwelcome. Similarly, Kjellgren and colleagues found in a questionnaire study that patients taking antihypertensives were prepared to tolerate unwelcome effects of limited severity in order to achieve perceived benefit.17 It seems therefore that patients' experience of palpable effects relates to more complex considerations than the effects' mere presence or absence. The acceptability of a ‘side effect’ to an individual patient depends not only upon whether it is unwelcome, but also upon its significance to that individual and the way that they balance it against reasons to take antihypertensives. This process may lead different individuals to different conclusions.
The interrelationship described between patients' reactions to palpable effects and reasons to take medication has implications for research exploring the link between side effects and medication use. Studies that identify the simple presence or absence of side effects, without taking account of the way that patients perceive them and weigh them up, may fail to specify side effects in the terms that are significant for patients.
If patients may accept unwelcome side effects from their antihypertensives, balancing them against personally meaningful reasons to take medicines, then clinicians and their patients can explore this avenue, before abandoning a medication in the face of unwelcome effects. This may increase options when trying to achieve target blood pressures to maximise clinical benefit: one of the reasons to accept unwelcome effects that patients themselves mentioned.
Patients in this study discussed some reactions to unwelcome side effects with their doctor more commonly than others. All discussed stopping medication, but only about half discussed continuing tablets unchanged or taking tablets differently. Very few discussed countering side effects without adjusting tablet taking. These proportions need cautious interpretation in a qualitative study and are derived only from patients persisting with medication. Nevertheless, the finding that much coping with unwelcome effects goes on without medical involvement supports the notion that many patients actively manage their medicines themselves.5 If clinicians wish to take these experiences and patients' consequent actions into account when planning treatment, they are likely to have to explore them actively.
This is significant for those who wish to take a concordant approach to prescribing, in which patients are involved in decision making.18 Discussion with patients of the way that these considerations work in their particular case will permit clinicians to establish which palpable effects their patients find unacceptable and why, to explore reasons for patients modifying the way they take their tablets and to offer advice tailored to an individual's experience. It may be that such advice need not necessarily involve a change of tablets in the face of unwelcome effects, should patients opt to accept them.
Declaration
Funding: JB was able to undertake the study through the award of a Health Services Research Fellowship from the Anglia and Oxford Health Authority and an Honorary Research Fellowship in the Guys, Kings and St Thomas's Department of General Practice and Primary Care. JB was provided with research expenses through a grant from the Scientific Foundation Board of the Royal College of General Practitioners. NB received no funding for the study. She acted as JB's supervisor for the performance of this research, which was presented by JB for the degree of MD in the University of London in 2001.
Ethical approval: Cambridge Local Research Ethics Committee.
Conflicts of interest: none.
We are grateful to the patients and staff of East Barnwell Health Centre, Arbury Road Surgery and Lensfield Medical Practice, Cambridge, UK for permitting and supporting the study's conduct; to Dr R H King, Dr A Watson, Dr S Jones and Dr S Holmes for practical help; and to Professor AL Kinmonth for comments on the paper.
References
Bardage C, Isacson DG. Self-reported side-effects of antihypertensive drugs: an epidemiological study on prevalence and impact on health-state utility.
Kjellgren KI, Ahlner J, Dahlof B, Gill H, Hedner T, Saljo R. Perceived symptoms amongst hypertensive patients in routine clinical practice—a population-based study.
Morgan M. The significance of ethnicity for health promotion: patients' use of anti-hypertensive drugs in inner London.
Luscher TF, Vetter H, Siegenthaler W, Vetter W. Compliance in hypertension: facts and concepts.
Dusing R, Weisser B, Mengden T, Vetter H. Changes in antihypertensive therapy—the role of adverse effects and compliance.
Boyle CM. Difference between patients' and doctors' interpretation of some common medical terms.
Nichter M, Vuckovic N. Agenda for an anthropology of pharmaceutical practice.
Benson J, Britten N. Patients' decisions about whether or not to take antihypertensive drugs: qualitative study
Kuzel AJ. Sampling in Qualitative Enquiry. In Crabtree BF, Miller WL (eds). Doing Qualitative Research. Newbury Park CA: Sage;
Morgan M, Watkins CJ. Managing Hypertension: Belief and Responses to Medication among Cultural Groups.
McMurray J, Northridge D, Bradbury A. The Cardiovascular System. In Munro JF, Campbell IW (eds). MacLeod's Clinical Examination. Edinburgh: Churchill Livingstone;
Svensson S, Kjellgren KI, Ahlner J, Saljo R. Reasons for adherence with antihypertensive medication.
Pound P, Britten N, Morgan M, Yardley L, Pope C, Daker-White G, Campbell R. Resisting medicines: a synthesis of qualitative studies of medicine taking.
Kjellgren KI, Ahlner J, Dahlof B, Gill H, Hedner T, Saljo R. Patients' and physicians' assessment of risks associated with hypertension and benefits from treatment.
Author notes
aUniversity Lecturer in General Practice, General Practice and Primary Care Research Unit, Institute of Public Health, University of Cambridge, Forvie Site, Robinson Way, Cambridge CB2 2SR and bProfessor in Applied Healthcare Research, Institute of Health and Social Care Research, Peninsula Medical School, St Lukes Campus, Exeter EX1 2LU, UK