Abstract
OBJECTIVE: There is no proven primary care treatment for patients with medically unexplained symptoms (MUS). We hypothesized that a long-term, multidimensional intervention by primary care providers would improve MUS patients’ mental health.
DESIGN: Clinical trial.
SETTING: HMO in Lansing, MI.
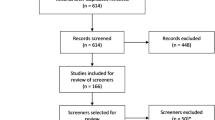
PARTICIPANTS: Patients from 18 to 65 years old with 2 consecutive years of high utilization were identified as having MUS by a reliable chart rating procedure; 206 subjects were randomized and 200 completed the study.
INTERVENTION: From May 2000 to January 2003, 4 primary care clinicians deployed a 12-month intervention consisting of cognitive-behavioral, pharmacological, and other treatment modalities. A behaviorally defined patient-centered method was used by clinicians to facilitate this treatment and the provider-patient relationship.
MAIN OUTCOME MEASURE: The primary endpoint was an improvement from baseline to 12 months of 4 or more points on the Mental Component Summary of the SF-36.
RESULTS: Two hundred patients averaged 13.6 visits for the year preceding study. The average age was 47.7 years and 79.1% were females. Using intent to treat, 48 treatment and 34 control patients improved (odds ratio [OR]=1.92, 95% confidence interval [CI]: 1.08 to 3.40; P=.02). The relative benefit (relative “risk” for improving) was 1.47 (CI: 1.05 to 2.07), and the number needed to treat was 6.4 (95% CI: 0.89 to 11.89). The following baseline measures predicted improvement: severe mental dysfunction (P<.001), severe body pain (P=.039), nonsevere physical dysfunction (P=.003), and at least 16 years of education (P=.022); c-statistic=0.75.
CONCLUSION: The first multidimensional intervention by primary care clinicians led to clinically significant improvement in MUS patients.
Similar content being viewed by others
References
deGruy F, Columbia L, Dickinson P. Somatization disorder in a family practice. J Fam Pract. 1987;25:45–51.
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
Smith RC, Gardiner JC, Lyles JS, et al. Exploration of DSM-IV criteria in primary care patients with medically unexplained symptoms. Psychosom Med. 2005;67:123–9.
Escobar JI, Waitzkin H, Silver RC, Gara M, Holman A. Abridged somatization: a study in primary care. Psychosom Med. 1998;60:466–72.
Bridges KW, Goldberg DP. Somatic presentation of DSM III psychiatric disorders in primary care. J Psychosom Res. 1985;29:563–9.
Smith RC, Lein C, Collins C, et al. Treating patients with medically unexplained symptoms in primary care. J Gen Intern Med. 2003;18:478–89.
Lyles JS, Hodges A, Collins C, et al. Using nurse practitioners to implement an intervention in primary care for high utilizing patients with medically unexplained symptoms. Gen Hosp Psychiatry. 2003;25:63–73.
Smith RC, Korban E, Kanj M, et al. A method for rating charts to identify and classify patients with medically unexplained symptoms. Psychother Psychosom. 2004;73:36–42.
Ware JE Jr., Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston: The Health Institute, New England Medical Center; 1994.
Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. Br Med J. 2002;324:819–23.
Smith RC. Patient-Centered Interviewing: An Evidence-Based Method. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2002.
Sharpe M. Cognitive behavioural therapies in the treatment of functional somatic symptoms. In: Mayou R, Bass C, Sharpe M, eds. Treatment of Functional Somatic Symptoms. Oxford: Oxford University Press; 1995:122–43.
Spitzer RL, Williams JBW, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care—the PRIME-MD Study. JAMA. 1994;272:1749–56.
Smith RC, Lyles JS, Mettler J, et al. The effectiveness of intensive training for residents in interviewing. A randomized, controlled study. Ann Intern Med. 1998;128:118–26.
Katon W, Von Korff M, Lin E, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression—a randomized trial. Arch Gen Psychiatry. 1999;46:1109–15.
Sartorius N. Composite International Diagnostic Interview (CIDI)—Core Version 1.1. Copyright World Health Organization.
Ware JJE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey—Manual and Interpretation Guide. Boston: The Health Institute, New England Medical Center; 1993.
Von Korff M, Ustun TB, Ormel J, Kaplan I, Simon GE. Self-report disability in an international primary care study of psychological illness. J Clin Epidemiol. 1996;49:297–303.
Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Chibnall J, Tait R. The Psychosomatic Symptom Checklist revisited: reliability and validity in a chronic pain population. J Behav Med. 1989;12:297–307.
Spielberger CD, Gorsuch RL, Lushene PR, Jacobs GA. State-Trait Anxiety Inventory (Form Y) (“Self-Evaluation Questionnaire”). Palo Alto, CA: Consulting Psychologists Press Inc; 1983.
Smith RC, Lyles JS, Mettler JA, et al. A strategy for improving patient satisfaction by the intensive training of residents in psychosocial medicine: a controlled, randomized study. Acad Med. 1995;70:729–32.
Escobar JI, Swartz M, Rubio-Stipec M, Manu P. Medically unexplained symptoms: distribution, risk factors, and comorbidity. In: Kirmayer LJ, Robbins JM, eds. Current Concepts of Somatization: Research and Clinical Perspectives. Washington, DC: American Psychiatric Press Inc; 1991:63–78.
Hall JA, Roter DL, Milburn MA. Illness and satisfaction with medical care. Curr Dir Psychol Sci. 1999;8:96–9.
Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82.
Barsky AJ, Ahern DK. Cognitive behavior therapy for hypochondriasis—a randomized controlled trial. JAMA. 2004;291:1464–70.
Torrance GW, Siegel JE, Luce BR. Framing and designing the cost-effectiveness analysis. In: Gold MR, Siegel JE, Russell LB, Weinstein MC, eds. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996:54–81.
Lin E, Katon W, Simon G, et al. Achieving guidelines for the treatment of depression in primary care: is physician education enough? Med Care. 1997;35:831–42.
Kroenke K. The interface between physical and psychological symptoms. Primary Care Companion. J Clin Psychiatry. 2003;5(Suppl 7):11–8.
Henningsen P, Zimmermann T, Sattel H. Medically unexplained physical symptoms, anxiety, and depression: a meta-analytic review. Psychosom Med. 2003;65:528–33.
Escobar JI, Gara M, Silver RC, Waitzkin G, Holman A, Compton W. Somatisation disorder in primary care. Br J Psychiatry. 1998;173:262–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by NIMH grant MH 57099. Orally presented as a research abstract at the annual meetings of the Society of General Internal Medicine (May 2004), the American Academy on Physician and Patient Research Forum (October 2004), and the Academy of Psychosomatic Medicine (November 2004).
Rights and permissions
About this article
Cite this article
Smith, R.C., Lyles, J.S., Gardiner, J.C. et al. Primary care clinicians treat patients with medically unexplained symptoms. J Gen Intern Med 21, 671–677 (2006). https://doi.org/10.1111/j.1525-1497.2006.00460.x
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1111/j.1525-1497.2006.00460.x